Could You Have SIBO?
Featuring
Julie Ann Davey, RN, MSN, ANP-C, ACNP-C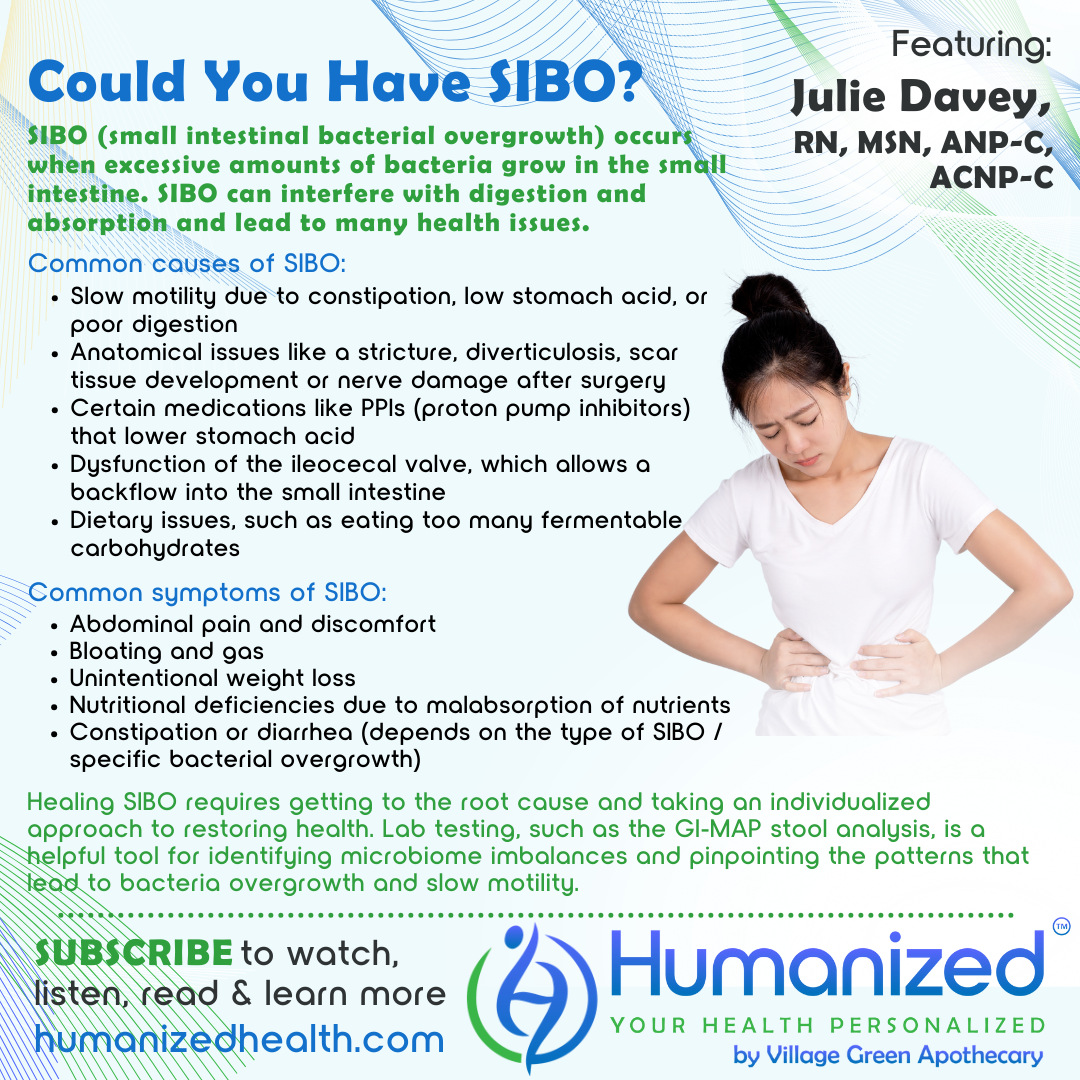
WATCH
LISTEN
READ
David Stouder: Welcome everyone to the Humanized podcast. This is all about personalizing your health. I’m your guest host today, Dave Stouder. Rebekah Kelley will be back with us next time. And we have an interesting topic today. Could you have SIBO? Do you know what SIBO is? S-I-B-O? Well, we’re going to find out because we have nurse practitioner, Julie Davey. And before I introduce her, I just want to remind you that if you go to HumanizedHealth.com, we have so many wonderful podcasts with the thought leaders of the natural foods movement. It’s all about personalizing your health. You’ve got videos, you’ve got audio, you’ve got transcripts, and we definitely want to thank our lead sponsor Village Green Apothecary for making this all possible.
Now, Julie’s been on Humanized Health several times. You’ve almost got an ongoing library of information about natural health because of our interviews with Julie. She’s a nurse practitioner with over 25 years of experience. She’s very passionate about educating others on the power of food and natural medicine to heal the body. Her clinical practice primarily focuses on GI health, where she utilizes specialty lab testing to help clients get to the root cause of their symptoms. She creates tailored protocols and empowers individuals with the necessary tools to have a healthy and vibrant life. And from all the many podcasts we’ve done with you, Julie, I certainly think this is an apt description and welcome to Humanized Health.
Julie Davey: Well, thank you so much. Thank you for having me again. This is such a popular topic. So, I’m excited that we’re going to cover this today.
David Stouder: Yeah, we certainly, here in the health food stores, hear a lot about SIBO and read a lot about it, but it may be completely unknown to most people. So, what exactly is S-I-B-O, SIBO?
Julie Davey: Okay, so SIBO stands for small intestinal bacterial overgrowth.
So, basically, the small intestines typically contain a relatively low number of bacteria. Now the colon, or the large intestine, typically contains more. And so, sometimes these bacteria can migrate back into the small intestine and then they become overgrown and that’s when we start to see a lot of issues.
Now, you may be asking, “Why does this even happen? Why would someone actually develop SIBO?” So, there are a couple of different reasons. First, is the motility is somehow altered, meaning that things are moving slower through the digestive tract. So this could be just from constipation. This could be from having low stomach acid. That’s a very common issue, especially with some specific bacteria that we can see overgrown like H. pylori. That’s one that probably many of the listeners have heard of.
David Stouder: If I may just ask a quick question, because I think we talked about this before, but since you mentioned it, aren’t a great majority of people with reflux experiencing low stomach acid?
Julie Davey: Yes, absolutely.
David Stouder: I just want to make that point.
Julie Davey: Yep. It’s very counterintuitive, but yes, a large number of people, the majority of people, in fact, who have acid reflux, it’s actually a low acid problem that’s causing this maldigestion and food to sit on the stomach longer. And then it refluxes back into the esophagus. So, it’s often not a high acid problem, which is what we’ve always been led to believe. So, I’m glad you pointed that out.
Some other things that can alter this motility could be things like you’ve had some type of surgery and there’s been some scar tissue development, some nerve damage, things like that. So, we always have to be thinking and kind of investigating when we’re looking for a root cause because that’s the goal, that’s how we correct most any issue is by getting to the root cause. It could be an anatomical issue like a stricture, or you could have some diverticula that actually create these pockets where bacteria can accumulate and then get overgrown. Certain medications – things like those PPIs (proton pump inhibitors), that actually lower the stomach acid, so then things don’t digest as well. Often motility is slower when we have that lower acid. There can be dysfunction of something called the ileocecal valve, and that’s the valve that is in between the large intestine and the small intestine. And if that valve is not working properly and preventing this backflow into the small intestine, if it’s dysfunctional, then that can be a cause of SIBO. It can be a dietary issue. Sometimes people are eating too many carbohydrates, too many fermentable carbohydrates, and that can cause these bacteria to get overgrown. So, those are just kind of some of the most common reasons that you could develop SIBO.
If you’re thinking, “Well, how would I know if I potentially had SIBO?” Some of the biggest symptoms that we see are abdominal pain and discomfort, bloating, lots of bloating and gas. You can have constipation or diarrhea because there are different types of SIBO and it’s really dependent upon the type, and the type of bacteria that are causing the issue as to whether or not you have constipation or diarrhea. You can have nutritional deficiencies because you get a lot of malabsorption of nutrients. And then sometimes people will also have weight loss. So, those are probably the most common symptoms that we see in people with SIBO.
David Stouder: Well, I wonder now, I’ve only probably heard the term SIBO last couple of years or so. The way you describe it, this sounds like this has been an underlying issue for a long time for a lot of people, and we’re only now just realizing it. Is that perhaps the case?
Julie Davey: Yes, I think so. And I think there’s just a lot more awareness around it now. And, it’s kind of one of those buzz words, right? That kind of get out there and then people start to hear more about it and then search more, and there’s a little more awareness around it.
David Stouder: Well, how do we actually diagnose this? If I had some of these discomforts, and a lot of people do, then if I came to you, how would you determine if I had something else going on or if I had SIBO?
Julie Davey: Well, I love that you asked the question that way. Because if you came to me, I would run a stool test on you called a GI-MAP, because that is going to give me much more information than what your standard classic test for SIBO is, and that is a breath test. So, if you just went and you said, let’s say you went to a practitioner and you said, “Hey, I want to know if I have SIBO,” then the classic test for that would be this breath test. And so basically what happens is, you have to blow into this bag, multiple times over, it’s like a two to three hour period every 15 to 30 minutes. So, you do a baseline test, then you ingest this carbohydrate solution that’s either lactose or glucose. And then what happens is if SIBO is present, those bacteria there in the small intestine will start to metabolize this carbohydrate and then that produces the gasses like hydrogen or methane.
So, there is a hydrogen type SIBO, there’s a methane type SIBO, and that’s what will be detected on the breath test. So, is that helpful or not? Well, in my opinion as a practitioner, it’s not near as helpful as knowing, okay, if you have SIBO, why do you have SIBO? So, that’s the whole goal is to get to the underlying root cause. And that’s why I like to do a stool test. I don’t even do breath tests because, honestly, it doesn’t necessarily matter to me if you have SIBO if I don’t know what the cause of the SIBO is. And on the stool test, it’s not diagnostic for SIBO, but we get these patterns that we see. So, if certain bacteria are overgrown, and those bacteria we know are some of them are hydrogen producing, some of them are methane producing, and you have these classic symptoms of SIBO, then I can pretty much say, yes, you most likely have SIBO, but the reason you have it is maybe we know you have H. pylori, or we know you have staph or strep overgrowth. So, that’s what I’m going to target because that’s the ultimate fix for it. Hopefully that made sense, Dave.
David Stouder: Well, it does. I see people come in with lab tests from doctors (a different topic), but they’ll say “My liver enzymes are high.” Okay. Why? And no one knows. Is it mold? Is it a toxin? Is it the medication you took? Is it just you had a bunch of alcohol last night? And, to me, I can breathe into this bag and they can say, well, you know I see signs of an overgrowth, but yeah, I want to know more than that. You know, I really want to know, like you said, that it could be a lot of reasons why that’s happened to me. And of course, I’m assuming that if you knew it was diverticulitis or my medication or et cetera, then that would change the way that you would help me.
Julie Davey: Yes, absolutely. Getting to that root cause is really the only way to heal and improve for good. Otherwise, it’s just that typical bandaid approach that we see all of the time.
David Stouder: Okay. Now, if I may, since you’re here, I’m going to ask you a question and I think it’s a pretty pertinent one. You know, normally I would say, and I think this is pretty defensible, that sort of the two pillars of good digestion, in terms of perhaps supplements, would be enzymes and probiotics, just generally. If you have good enzymatic reaction, good microbiome, things are fairly well, but I understand that we don’t really know necessarily how well to handle probiotics with SIBO because some could be very helpful and some might make the condition worse. Is, is that accurate?
Julie Davey: Yes, I would say that is definitely accurate. So, there are a couple of things – and this is one of the reasons that I like to have a stool test – if I see on the stool test that there is a pattern of slow motility, typically we see that when some of the good and commensal bacteria are overgrown. Then I know that if I give that person probiotics before I restore motility, they’re probably not going to feel very well. And that’s a very common pattern with SIBO. So, we don’t necessarily now exclude probiotics in a SIBO patient, but I think it has to be, really just like it should be, a very individualized approach. And, we know that some probiotics are better for SIBO patients. So, maybe something like a spore-based probiotic or one called Saccharomyces boulardii, which is a yeast-based probiotic versus some of your kind of general standard probiotics that are lactobacillus, bifidobacterium. Those type things tend to cause more symptoms and issues in SIBO patients. So, I would typically choose, again, spore-based or S. boulardii, something like that. But yes, that was a great question.
David Stouder: If you do the good testing so that you know the root cause, is there a good success rate in getting people back to a good stable place?
Julie Davey: Yes, absolutely. So, this is what I see very often with SIBO, especially. People will come to me and say, “I’ve been tested for SIBO. I had it. I took antibiotics. I was feeling good. And then it came back. I got tested again, showed positive again.” So, that’s just kind of like a very classic thing that happens, and it’s because we didn’t address and find the root cause. So, if you just went to some practitioner, you had a breath test, they tell you you have SIBO, most likely what they’re going to do is give you an antibiotic, one called Rifaximin, that’s like the most common thing to take for SIBO. And, there’s just a high failure rate with that because again, the root cause is often not addressed there, so it’s going to come back most likely.
Now, there are some other things that often are recommended and that are good. Things like what we call a Low-FODMAP diet. And that’s basically just a diet that reduces the consumption of these fermentable carbs. Because when we’re consuming those type things, then these bacteria in the small intestine really just have a party. They just feed and grow and multiply off of it and produce these gases and that’s when we have lots of symptoms. So, Low-FODMAP diet, that’s not a long term solution. Until we address the root cause that can help with some of the symptoms. So, that may be done. Then also, sometimes you’ll see some motility agents given some prokinetics that, again, if you have more of the slower motility that can help, but I would just say to everyone listening, the ultimate fix is to get to that root cause.
David Stouder: Well, yeah, I think in situations like this, certainly our symptoms are the signs of something’s wrong and many of them are uncomfortable. I tell people, don’t focus on fighting stomach acid, focus on restoring digestive integrity and digestive function. And I think with all these things, yeah, if you have acid, if you’re constipated, if you have diarrhea, you want to resolve that, but you don’t want to stop there. There’s a lot of things that can resolve those symptoms that, as you say, don’t get to the root cause and don’t restore digestive integrity. So, for people out there suffering with SIBO or just having an issue, and maybe this is ringing true to them, they’ve gone, they got antibiotics two or three times. And don’t worry folks, we’re going to give you Julie’s website so you can get in touch with her. You do Telemedicine, right?
Julie Davey: Yes, I do. I’m in Georgia.
David Stouder: Georgia. Okay. South of us anyway. So I’ll be giving her website out here in a moment if you’d like to deal directly with Julie, you certainly can. But, if you do go to a practitioner, then you would say you want somebody that’s going to do like a GI-MAP testing. I think there are a couple different ones out there, so that they can really see the nature of your SIBO, what is overgrown, probably why, and then you have a better chance of restoring yourself to good health.
Julie Davey: Yes, absolutely.
David Stouder: All right, well, that’s good. And now I’m going to give out your website if you would like to get in touch with Julie Davey, and I urge you to do so. I just want to say something, I think we’ve done about 9 or 10 episodes with you, Julie. And it’s interesting, I guess it’s not unexpected, but no matter what digestive topic we talk about, I want people to know that we don’t really go over notes as far as, well, what are you going to say. I feel very free to ask Julie questions and she has good answers because she knows what she’s doing.
So, here’s her website, www.JulieAnnWellness.com and that’s J-U-L-I-E-A-N-N, not with an E, JulieAnnWellness.com. And you’re welcome to reach out to her. I would remind you that you can go to Humanized Health and we’ve got all kinds of videos and podcasts, and I think we’re up to 8 to 10 episodes with our guest today, Julie Davey.
So, thanks again, I learned a lot about SIBO. I’m going to be more helpful here in Village Green Apothecary when people ask me questions. Thanks for being on the program today.
Julie Davey: Thank you so much for having me.









