FODMAPs and Their Connection to IBS and Digestive Issues
Featuring
Julie Matthews, CNC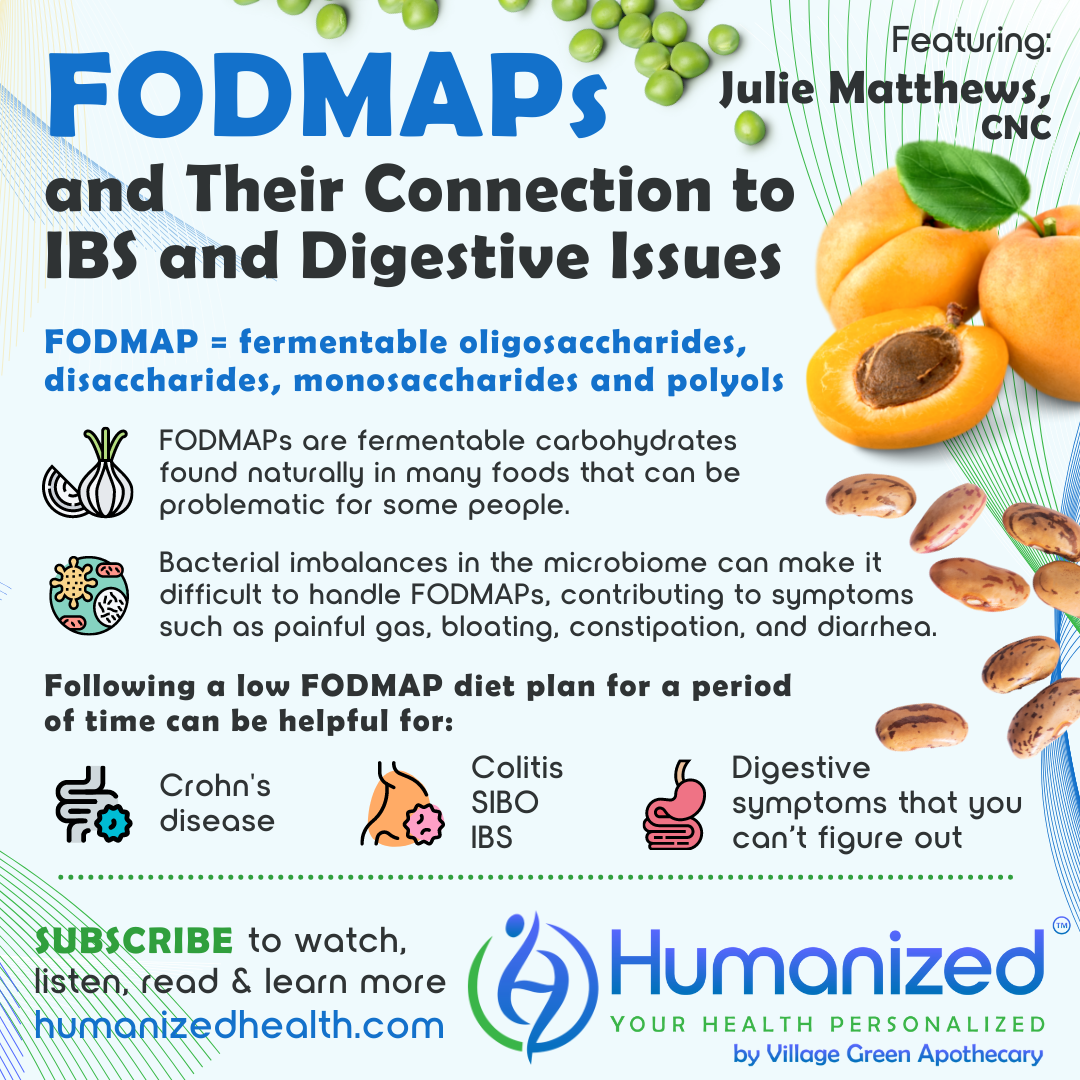
WATCH
LISTEN
READ
Rebekah Kelley: Welcome to the Humanized podcast, all about personalizing your health. I am your host, Rebekah Kelley, and today we’ll be discussing FODMAPs and Their Connection to IBS and Digestive Issues, with Julie Matthews. Before I introduce Julie, I want to remind everyone to subscribe to all of our variety of casts in audio, video and transcription at HumanizedHealth.com. I’d also like to thank our lead sponsor, Village Green Apothecary at MyVillageGreen.com
A little bit about Julie Matthews. She is a Certified Nutrition Consultant and published researcher specializing in complex neurological, digestive and immune conditions, most notably autism. She is the author of the award-winning book, Nourishing Hope for Autism, and co-author of a study, “Proving the Efficacy of Nutrition and Dietary Intervention for Autism,” published in the peer reviewed journal Nutrients. Julie’s approach is based on the personalized nutrition needs of each person and stems from her 20 years of clinical nutrition experience and research. Her methodology of bio-individual nutrition helps individuals and practitioners who work with a wide range of disorders for adults and children improve health and healing.
Julie, thank you so much for being here with us.
Julie Matthews: Thanks, Rebekah. I’m really glad to be here.
Rebekah Kelley: So you practice bio-individual nutrition. Can you tell us what that is?
Julie Matthews: Yes, so bio-individual nutrition is… bio-individuality is really biochemical individuality. So it’s looking at an individual on their personal level of what’s going on with their biochemistry in their body. So it’s really personalized nutrition and it’s really just looking at what’s going on for them underneath and helping to really individualize it for the person. And so I would get very detailed into, what is their biochemistry, what health conditions do they have, what symptoms, reactions, all of those things, so that we can create a customized diet and nutrition plan that’s very specifically for them.
Rebekah Kelley: Awesome. So what is a low FODMAP diet?
Julie Matthews: So it is, FODMAPs is an acronym for a variety of different fermentable carbohydrates. So, things like fructose and oligosaccharides, disaccharides, and polyols, things like that. Monosaccharides. And different ones are problematic for different people. Some of them are monosaccharides, but there’s a challenge absorbing them. In other cases with disaccharides, it’s a problem breaking them down into their primary components, their monosaccharides. Or it could be these longer chain carbohydrates, things like what’s in beans or onions, these longer chains. And these fermentable carbohydrates have done to them what it sounds like, they get fermented, and they are fermented by bacteria. So when we don’t have the right bacteria and microbiome in the right place, then when we ferment, when our microbiome ferments these carbohydrates, it can create a lot of symptoms – gas, pain, bloating, diarrhea, constipation, depending on the person.
Rebekah Kelley: It sounds like from some of the things that you’ve listed, that these actually can be considered healthy foods, like beans are considered healthy foods, but it’s just that it just doesn’t work with that individual. It creates problems for that individual.
Julie Matthews: Absolutely. And some of the tricky part to that is that some of the best foods for feeding the microbiome, like beans, are some of the things that cause a problem for certain people. And so it gets a little tricky because some people might need to work on promoting some of the beneficial bacteria, but when they try to do that, they get symptoms. And so sometimes dysbiosis isn’t always that you have pathogens. It could be, you have too much of a good bacteria, but in the wrong place, or something like that. So, absolutely, these are good foods. We don’t necessarily want to limit them for everybody, but we do need to maybe reduce them or limit them maybe for a period of time, or for certain ones for certain individuals, because they just don’t work for them.
Rebekah Kelley: So that kind of ties into the next question. When is a low FODMAPs diet beneficial?
Julie Matthews: Usually I find it most beneficial when someone is dealing with digestive issues. There are some really good studies that have been done on Crohn’s and colitis out of Australia looking at these particular foods, we’ll call them foods, or these compounds in foods. And so we’ve seen a lot of good research on that. There’s also information related to a lot of practitioners using this diet with SIBO, small intestinal bacterial overgrowth, where we’re saying that there’s the good bacteria, but there’s too much of it in the small intestine. The bacteria that’s supposed to be more in the colon is more in the small intestine and that can create a lot of these symptoms we’re talking about.
So I tend to like to look at that diet when someone’s dealing with digestive issues that they can’t figure out, or they’re looking for one of the potential diets that might be able to help with digestive issues. So lots of those symptoms we talked about – gas, bloating, diarrhea, constipation. It might be alternating back and forth, so it’s hard for them to figure out what’s going on. But I often find a lot of painful gas, kind of trapped gas, those sorts of reactions.
Rebekah Kelley: So you mentioned… but what’s the research on the low FODMAP diet?
Julie Matthews: Yeah, so, we go into some of that. I’m just going to write down for myself some notes as we go here. The research really should, looking into it… the good thing about this diet is that we see some of that research. So, we could dive into a little bit of it. I think that there’s two things that are good and important here. One is kind of the anecdotal evidence of what practitioners… there’s some great practitioners out there. Dr. Alison Siebecker doing great work, and Dr. [Mark] Pimintel doing work with SIBO and looking at diets, like the low FODMAPs diet, and doing their own clinical work and clinical research in that area, whether it’s published or not. Some is, some isn’t. There are different practitioners doing some really great research and really looking at IBS, inflammatory bowel issues, or irritable bowel issues – but also inflammatory bowel conditions like what I was saying, colitis, Crohn’s disease, and there’s some really good information on that. Some people do combine the diet with other diets. So that’s kind of where I like to think about the bio-individual nutrition aspects.
So for me, doing what I do, I might bring these low FODMAP principles into a diet plan, into a personalized diet plan with somebody. So I might say, okay, this person is having these digestive issues, maybe we’ll start with the low FODMAP diet. Maybe that’s not enough. Then I might bring in some of the principles of something like a specific carbohydrate diet, where, because what’s interesting in these two diets, FODMAP removes the sort of medium chain carbohydrates, whereas the specific carbohydrate diet removes disaccharides and long chain polysaccharides, like starches. FODMAPs brings in monosaccharides, a little disaccharides, but then also these medium chains that are not addressed in this other diet.
So I think it’s really sometimes beneficial to combine diet principles and maybe they need to do two diets or maybe they need to bring in a few principles from this one diet into another. Looking at some of that in terms of studies and things, usually the diet will be done removing all the food categories.
But the thing about the low FODMAPs diet is not everybody reacts to all the categories. Some people we know in the research with autism, some people have carbohydrate digesting enzyme problems, and some people have fructose malabsorption. I know, I tend to do a lot with autism, so I know that research off the top of my head. And so for them, they might have more of this issue with FODMAPs, whereas somebody else might have more of an issue with something else. So again, it’s bringing in that personalized aspect. With that research, when we kind of step beyond it, we go kind of more into the clinical setting, we then might want to see, okay, did removing those FODMAPs help? But then on a clinical perspective, we want to look at which ones do they need to avoid. Some people might just have more of an issue with the oligosaccharides, for example, and then just need to really avoid the beans and things. Or they might need to avoid some of the fructo oligosaccharides in probiotic supplements, cause those really get them. Other people might have more of an issue with the fructose and those things. So it’s, again, even within a FODMAPs diet, I feel like we want to do that bio-individual aspect of it because we don’t always need to avoid all of them all the time.
Rebekah Kelley: Wow, thanks, Julie. Those are really valuable insights. Julie Matthews can be found at www.NourishingHope.com. Let me remind you to subscribe and get access to all Humanized videos, podcasts and transcriptions from all of our thought leaders on personalized health at HumanizedHealth.com. Thanks so much for being with us, Julie.
Julie Matthews: Thank you.







