Important Lab Tests for Trauma Recovery
Featuring
Aimie Apigian, MD, MS, MPH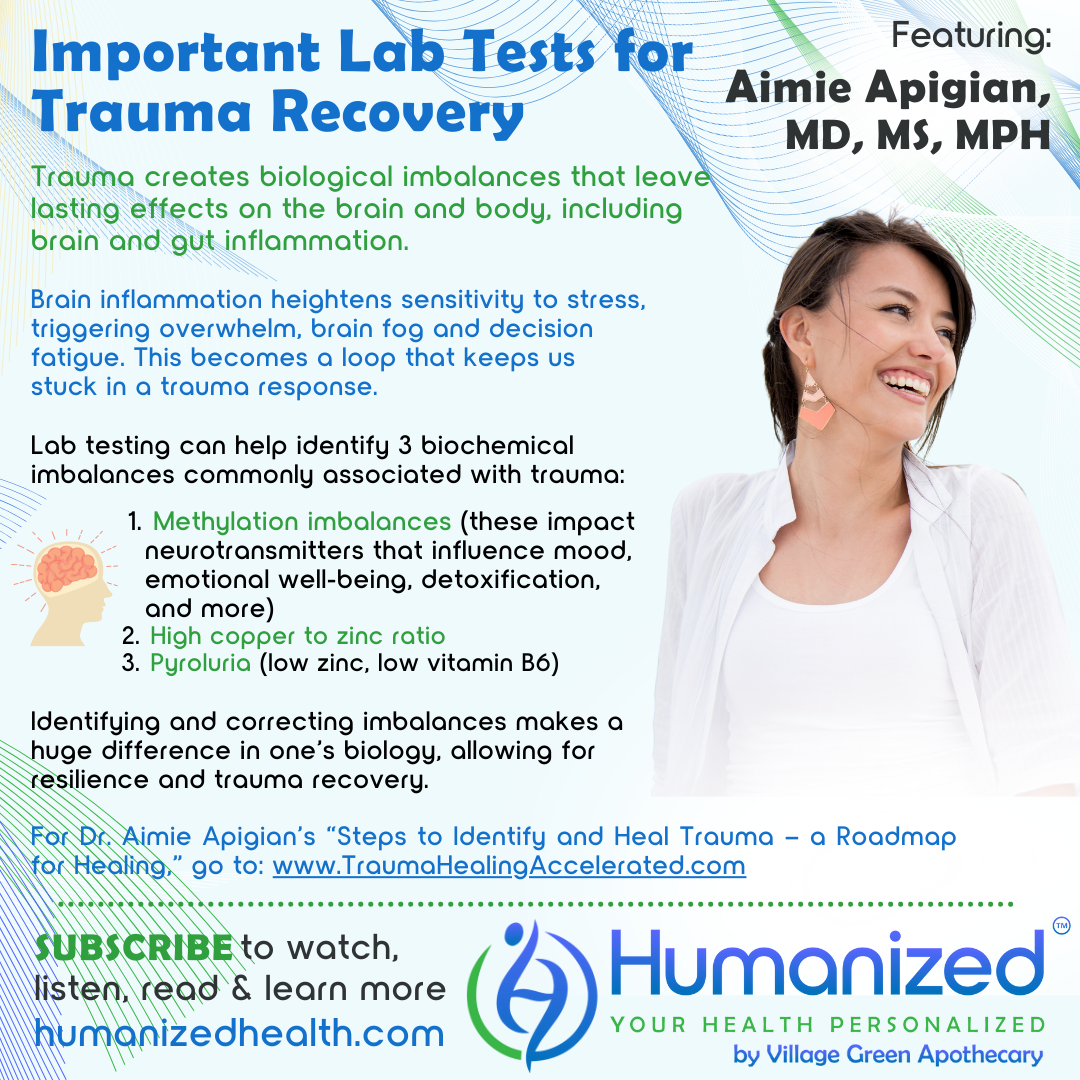
WATCH
LISTEN
READ
Rebekah Kelley: Welcome to the Humanized podcast, all about personalizing your health. I’m your host, Rebekah Kelley, and today our topic will be Important Lab Tests for Trauma Recovery with Dr. Aimie Apigian. Before I introduce Dr. Aimie, I want to remind everyone to subscribe and get all the other varieties of casts in audio, video and transcription at HumanizedHealth.com. I’d also like to thank our lead sponsor, Village Green Apothecary, at MyVillageGreen.com.
A little bit about Dr. Aimie. She is a double board-certified medical physician in both preventative and addiction medicine. She holds a double master’s degree in biochemistry and in public health. She’s a leading medical expert on addressing stored trauma in the body through her signature model and methodology, The Biology of Trauma, a new lens that courageously up-levels the old methods of trauma work in medicine by reverse engineering trauma’s effects on the nervous system and body on a cellular level. Dr. Aimie specializes in trauma, attachment and addictions after having personal experience in fostering, parenting, adopting, and then having her own health issues that were a result of childhood and life experiences. In addition to her medical studies that have included functional medicine certification, she has sought out trauma therapy training since 2015. Additionally, Dr. Aimie founded a nonprofit called Family Challenge Camp and developed and ran weekend intensives for families with children who have experienced attachment trauma. She is currently the founder and CEO of Trauma Healing Accelerated, where she bridges the two worlds of functional medicine and trauma therapy with a mission to help accelerate adults’ healing journey by addressing the biology of trauma that keeps stored trauma stuck in the body, mind and spirit. Her provider certification course teaches providers to do the same for their clients.
And as always, Dr. Aimie we love having you here. You provide such a great holistic perspective. So thank you.
Aimie Apigian: Thank you, Rebekah. I’m excited for this conversation today.
Rebekah Kelley: We always have such a good time. And when you explain things, I’m always like, that makes so much sense, right?
Aimie Apigian: The expressions on your face – you start to get pensive and then it’s like the dots start connecting and light bulbs go off. And I love watching you in that process.
Rebekah Kelley: And I’m so excited for our listeners, too, to be able to bring this message to them, if there’s something here that can help them with how they personalize their own health experience, right? Since we have Humanized Health.
So anyway, let’s jump right in. If you can talk to us and introduce us to how trauma creates biological imbalances in the brain and the body.
Aimie Apigian: Yeah. So I think that an important place for me to start would be that there’s a difference between stress and trauma. So we can go through hard things in life and they’re not necessarily trauma. They may just have been stressful. And the difference between stress and trauma is the brain and body’s ability to bounce back. And so if we go through a stress, we can recover and we bounce back. But if we go through something that’s really a trauma, that crosses a line. And that line is what leaves lasting effects. It’s like footprints that don’t go away. And those footprints are now evident in our brain, our brain chemistry, brain inflammation, brain neurotransmitters, and the body as well.
And so when we look back at our life, we can look for those times that were overwhelming to us. A time maybe that we felt all alone, unsupported and overwhelmed with it all. Maybe it was a time that things were just coming at us too much too fast and they felt too big, and we just felt like we wanted to curl up into a ball. We wanted to go back to bed. Those were the times that our body actually went into a trauma response. And by the body, there’s a specific aspect of our body that goes into a trauma response, and that is actually mediated by what we call the autonomic nervous system. So we have the central nervous system, which is our brain, our spine – but we have the autonomic nervous system, and that is really where it leaves its footprints when a trauma happens. And again, by trauma, my definition is anything that for any reason at that time in our life overwhelmed us. And by overwhelmed us, I mean, overwhelmed our autonomic nervous system, overwhelmed its ability to stay in the stress response, and it got overwhelmed and it crossed that line into the trauma response.
When we look at what are those footprints, then, that happen in the autonomic nervous system that leave the lasting effects on our brain and on our body, it’s changing the operating system. And when we understand the three different states of the autonomic nervous system, we can see the three different operating systems. So the autonomic nervous system, I think most people know this, but as a brief review, it’s what keeps us alive. And so it’s what keeps our kidneys working, filtering out the blood, creating urine. It’s what keeps our digestive system working, heart beating, lungs, breathing. But it’s not just doing that. It’s telling our heart how fast to beat. It’s telling our lungs how fast to breathe, how deep to breathe, how shallow to breathe in this moment, given what we’re experiencing.
And so being able to just say, oh, well, the autonomic nervous system keeps us alive and makes our body do all these things without us having to think about it, isn’t that wonderful? That is such a superficial view of this amazing, intelligent design of the body that tells it how to live life. Not just to live, not just to survive, but how to survive. And so when a body and an autonomic nervous system goes into that trauma response then, it changes the operating system to say, this is how we are going to live. This is how we are going to survive. And part of that is, we need to create some brain inflammation because there are clearly threats in our environment and we need to unleash that inflammatory cascade to protect ourselves, protect our neurons. And so there’s always brain inflammation that is a result of this trauma response.
And once you have brain inflammation, you have the primed microglia. And so now they are always more sensitive to stress and you’re able to only experience less stress, but have the same effect now of overwhelm and brain fog and decision fatigue, and what I call focus fatigue, like I just can’t seem to focus on anything for as long as what I used to be able to do.
And then when we look at the body, there are so many changes that happen as a result of this operating system saying this is how we’re going to survive. And the message specifically is, how we’re going to survive is by shutting down. And so it literally changes our mitochondria. It changes our metabolism. It changes our hormones. It changes… it changes everything because it’s telling our body, we need to operate on as little energy as possible. We just need to do enough to get by, but nothing more. We’ve got to save our energy. And I mean, that’s a whole operating system right there, because that’s very different from living life thriving.
That’s very different from living life feeling like, I’ve got this and yeah, there are problems, but I’ve got the resources, I’ve got the energy to tackle my problems. You’re going to feel all the time heavy and overwhelmed, and you’re going to feel like you’re having to push your body through life. And many people describe it as like, what’s wrong with my body? My body can’t keep up anymore. My body always feels heavy and tired, and I have to drink even more caffeine than usual in order to be able to do the same amount of things that I used to be able to do. And it progressively slowly gets worse over time. It builds, it accumulates. And so more and more people notice that they really aren’t able to do as much because their body just has accumulated the time spent in this trauma response and this way of living life.
So, I know that that was a lot, Rebekah, but there…
Rebekah Kelley: Well, it’s a deep subject and I have to take it in. As you’re just saying it like I’m, again, you said I’m putting the pieces together as you’re saying it and it’s making sense, but it’s something that you don’t hear every day, for sure. And the way you describe it, it just makes so much sense.
So when you say that our brain swelling, right, how, how do these imbalances or deficiencies, how does it make it difficult to heal? Like you were describing brain swelling, you’re describing that we’re tired, right?
I mean, are we stuck there, I guess is what it feels like you’re saying in a way, right? Like, how do you get out of that loop? How do you move on to the healing process?
Aimie Apigian: Yeah, and that’s exactly part of the problem, is that it does become a loop. It’s the brain Inflammation that the trauma response causes. And this is subclinical, so you’re not going to go to a physician and they’ll do an MRI and they’ll be like, oh my goodness, you have swelling in your brain This is subclinical Inflammation, neuroinflammation released by your immune cells in your brain called the microglia.
And even just that, what happens is that when our nervous system, now it’s our central nervous system, but it’s bathed in inflammation. Talk about a constant threat and danger, right? The, the inflammation is not something that the brain can even walk away from. Like if we have somebody in our life that is a threat, we can walk away, or we can hang up the phone, or we can not respond to their email, or tell them that we need to take a break. But you can’t do that when your neuron is bathed in inflammation. And so that becomes overwhelming. A brain in inflammation is a brain overwhelmed. And so that will now keep us, keep the autonomic nervous system in a trauma response, because it literally is getting this message of, we are overwhelmed. And this is an inescapable threat that we’re not able to fight off.
And so it becomes this loop and same thing with the other things in the body where the effects that trauma has on our biology become the biology that keeps us stuck in a trauma response.
Gut inflammation is another great example of that, where the trauma response shuts down the gut. So now your food is not being digested as well. You don’t have as much stomach acid, your protein breakdown for your food is not being released as much by your pancreas and now you have these larger elements of food passing down. You have the barriers that should be protecting your intestines are breaking down because that’s not what we should focus on when we are in survival mode, and you’ve got leaky gut. And that same inflammation from the leaky gut not only is going to travel up the vagus nerve to your brain and cause brain inflammation, but here we go again, we’ve got a whole nervous system inside of our gut called the enteric nervous system, and that is now bathed in inflammation. So you’ve got inflammation bathing your enteric nervous system. You’ve got inflammation bathing your central nervous system, and it’s this inescapable constant threat, and that is a body in overwhelm.
And so to think that it’s only emotional or psychological things that cause us trauma is not true. These are biology factors that will still create the same trauma response as if something severely emotional or psychological had happened.
Rebekah Kelley: And I think, I’ve heard so many times, well, you know, that’s in your head, right? Or that’s your thinking. And it’s like, oh yeah, I need to change my thinking, or I need to change… and you kind of then ignore what’s happening in the body, right? But when you connect it like that, it kind of means like everything is happening to you mentally and physically. And so therefore it can maybe be addressed a little bit differently than, oh that’s just in your head, right?
Aimie Apigian: It should be. I mean, to me, this is what gives me hope, right? Because it’s like, oh, I have more tools now. Rather than just the tools that we’ve had of, change your thinking, meditate, try harder.
Rebekah Kelley: Well, and speaking of tools though, you said before that you can’t necessarily go get an MRI, but this is about lab testing, right? Like that’s kind of the title here. So, why is lab testing such an important tool if it’s not the MRI? Then we would move into what is, what kind of testing is there? Can you talk to us about why lab testing is so important for trauma recovery? And then what are some of the lab tests that are essential?
Aimie Apigian: Absolutely. So as I teach the professionals in my training program now, there is a lens of the biology of trauma that informs everything that we do. The first step is identifying what are these trauma patterns in someone’s nervous system? How much time are they actually spending in a trauma response versus a stress response or parasympathetic? Are they even landing in parasympathetic? And so we actually have clients fill out what we call a nervous system tracker, where for 3 days, they are tracking their nervous system to tell us where they’re spending their time. Many of them, Rebekah, are actually waking up in a trauma response. What does that mean? That means that they’re waking up already overwhelmed. They don’t want to get out of bed. Like, their day hasn’t even started…
Rebekah Kelley: And that’s where the cups of coffee that you were mentioning before start, right? That probably starts it, right? And it probably still continues. Yeah.
Aimie Apigian: Exactly. And so being able to just recognize the pattern, what pattern am I seeing? Because then when I go and I get lab tests, I’m looking for how do these lab tests inform me for what’s driving this trauma response or stress response? And it gives me the idea of, I can identify the lowest hanging fruit when I understand the patterns first and then bring in the labs. Because if I just look at labs and I don’t know the pattern, I’m still kind of like, well, this seems complex. You have a lot of things going on, right? And that’s what people are told. There’s so much, and so here’s a 9-page summary of all the things you need to do, all the things you take. And I guarantee you that anyone who receives a 9-page summary of all of these things that they’re supposed to be doing, and if they’re struggling with a trauma response, they’re going to be overwhelmed by that.
Rebekah Kelley: Yeah, they’re already having a hard time getting through their day. So, 9 pages. And I’m assuming probably it’s not just coffee. They’re probably using sugar or other things to spike their energy. They might be using alcohol.
Aimie Apigian: Yes, all of that.
Rebekah Kelley: There’s going to be so many different things in order to help get yourself through your day.
Aimie Apigian: Whatever it takes to get through your day. Which is interesting. There’s all those coping mechanisms that people can look at of what do I do to just get through my day. And sometimes it also includes things like procrastination, where if I procrastinate, then all of a sudden I’m going to feel the adrenaline rush and I’m going to have the energy to get that thing done because I procrastinated long enough that it’s now a major stress and I have to get it done.
So it’s fascinating to see all the things that we’ve been able to come up with for how to just get through our day.
Rebekah Kelley: So what are… did you mention those specific lab tests? I was so focused on what you said. And then is there also a way that they can be personalized? Because my assumption is that different individuals are going to need different kinds of treatment, right? It’s not going to be the same.
Aimie Apigian: Exactly. Yes. And so once we find the patterns and identify the patterns, and by the patterns, I mean, are they going into this trauma response and how much time are they spending in this specific trauma physiology, then when we look at the labs, we can identify the lowest hanging fruit and personalize it for them based on what will make the biggest difference, the fastest.
And so for me, I am always starting with the biochemical imbalances. And there are three biochemical imbalances specifically that I’ve noticed will keep people stuck in this trauma response. It will create that loop that is really hard to get out of. And these three imbalances, again, not everyone has these, but these are so common that this is often where I am starting everyone when I see that they have this pattern of going into that trauma physiology.
And it includes methylation imbalance. And so, the methylation disorders, I mean, if we follow that down on all of the problems that they create in our biology, it will become very clear of why then that biology will keep us stuck. For one thing. I’ll just mention this, that those who have an under-methylation status, not all of them, but many of them can have low serotonin and low dopamine activity levels. Well, if you have low serotonin levels, everything feels a little gloomy, like everything just feels sad. And so what would be a stress for another person for you is going to be overwhelming sadness, overwhelming grief, overwhelming loneliness that you can’t seem to push through. Even the dopamine, right? Dopamine is that neurotransmitter that gives us the spark, the inertia to do something, the motivation, because I want this, this is pleasurable to me. And we find that with the low dopamine activities, people are doing things to get a dopamine hit. Even if that’s emotional eating, that happens a lot in order for us to get dopamine. Also the caffeine use will help with that dopamine. But if we don’t have that dopamine at normal levels, again, there’s just going to be no joy in life. Everything’s going to be flat. And so again, what for other people they would experience is maybe just something hard, for you, if you have low dopamine, it’s going to be even harder and likely going to push your body over into that line of overwhelm and the trauma response.
But then you can look at the detoxification system and methylation problems and the toxin overload that can happen. But even in under-methylation, there’s one other aspect that has become more, I would say well known in terms of how it contributes to the high anxiety. So under-methylators report a very high inner anxiety, even though on the surface, they look very calm. They look like they are cool, calm, and collected and got it all together. They are your driven people, your perfectionist. And yet they have such high inner anxiety. And what we’re finding is that that is actually due to the higher glutamate activity levels at the NMDA receptors. Well, you get high glutamate when you have brain inflammation. So activated microglia unleash all of this glutamate in the extracellular space, and now you’re having increased anxiety with brain inflammation. And so that is just one way in which this biochemical imbalance will keep you stuck in this loop of going into a trauma physiology.
The other ones are the copper to zinc [ratio]. So a copper excess, whether that’s a high copper to zinc ratio, or just by itself, a copper excess. And zinc deficiency would be another major thing. So that zinc really stabilizes and protects the nerves, the nervous system. And so if you’re low in zinc, and if you have something called pyroluria, which is the third biochemical imbalance, that you have a functional deficiency in zinc and B6, it’s like your nerves are raw. There’s no filter, there’s no protection. And so imagine going through life, even just stepping outside into the sunlight, and it’s like your reaction to that is exaggerated from other people simply because your nervous system is just so raw and sensitive, and so it’s so much more reactive. And walking out in the sunshine, and being around people, may be stress for someone else or may even be fun. And for you, for your system, because of these biochemical imbalances, it’s overwhelming to you. And all you want to do is just run away and be in a dark room all by yourself.
So there are these common biochemical imbalances that I’m seeing in this work with trauma that no matter where they’re coming in, if I’m seeing this trauma physiology, I’m asking them to get these lab tests specifically as a place to start, because they make such a big difference in the rest of the biology. When we have these, it’s almost like the rest of biology isn’t going to make much improvement either, no matter how much we throw at it, when this is still going to be driving a lot of that.
Rebekah Kelley: So this sounds very much like you’re talking about something that’s at the base of what’s happening within your biology, right? And it’s kind of hard to know that without these tests that you’re mentioning, right? But if someone wanted to get more information, they needed a little bit more help. They want to take the information that you’ve laid out today, I understand you have a free gift that could actually help them kind of get to that. Can you share that with us?
Aimie Apigian: Yeah. And I think that this is such important information for people to be able to look at, look at themselves, look at their traits, look at their personality and see, do I think that I have one of these, that I should get tested? Because if you do have one of these… I actually ended up having all three, Rebekah. I had all three at one point. And, and so being able to identify it and bringing in that support for yourself – what a difference that makes.
So what I would want for people to do is be able to read through the descriptions of what does it look like? How would I know if I might have one of these? And so I’ve laid all of that out in a guide on the three biochemical imbalances most commonly seen in the trauma physiology, so that people can look through those, see if one of them seems to resonate with them, like, yeah, that sounds like me, that sounds like me – just so that you can get that testing and be able to understand this level. Because again, if you have one of these, or two or three, it will make such a huge difference for your mood, for your resilience, for your ability to get through your days when you’re able to support your biology and not be struggling with these biochemical imbalances.
Rebekah Kelley: Thank you so much. So that’s going to be a downloadable guide. There’s a link that will be in this podcast for people to access. And, I just want to say thanks, Dr. Aimie, for your always valuable insights. Dr. Aimie can be found at www.TraumaHealingAccelerated.com. That’s trauma healing accelerated dot com. Let me remind you to subscribe and get access to all Humanized videos, podcasts, and transcriptions from all of our thought leaders, just like Dr. Aimie on personalizing your health at HumanizedHealth.com. Please come back and be with us again.









