Schizophrenia: The Underlying Biochemistry & How to Address It
Featuring
Albert Mensah, MD, BCIP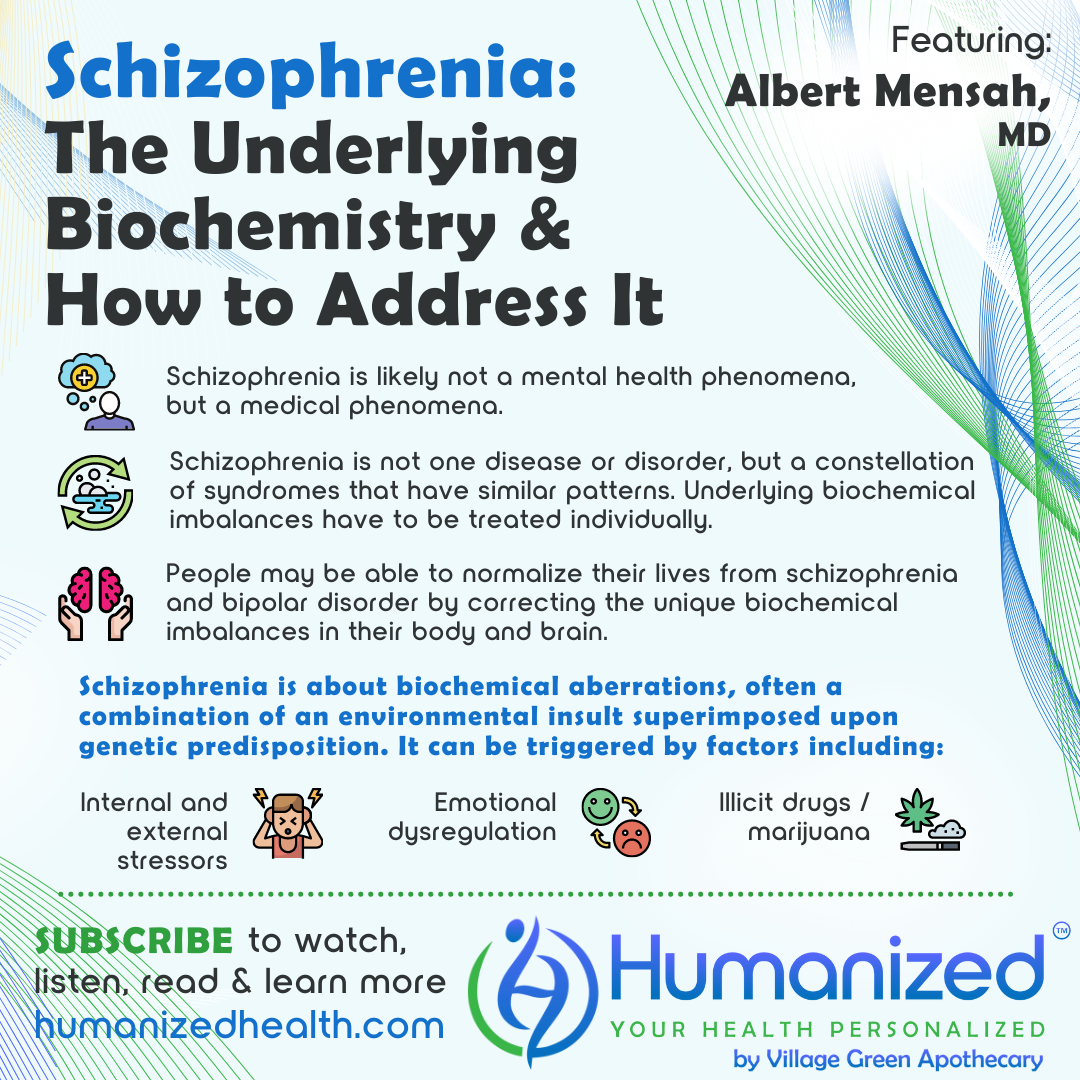
WATCH
LISTEN
READ
David Stouder: Welcome to the Humanized podcast. It’s all about personalizing your health. I’m your host, Dave Stouder. Now today we’ll be discussing Schizophrenia with Dr. Albert Mensah. And before I introduce Dr. Mensah, I want to remind everyone to subscribe, to get all of our variety of casts – audio, video transcript – at HumanizedHealth.com. Very simple. I’d also like to thank our lead sponsor, Village Green Apothecary. You can find them at MyVillageGreen.com, as well.
Now I’m going to tell you a little bit about our guest today, and do want you to know that at the end of the podcast, we’ll let you know his website so you can get in touch with him, as well.
Dr. Albert Mensah specializes in treating mental health disorders through biochemical lab testing and individualized targeted nutrient therapy. He’s co-founder of Mensah Medical in Warrenville, Illinois, an integrative health clinic, as well as the Mensah Research Institute, a not-for-profit organization dedicated to conducting, supporting and presenting research that provides scientific evidence of the efficacy of targeted nutrient therapy.
Well, Dr. Mensah, we’re going to talk about, I think, a condition, schizophrenia, that most people don’t associate with nutrient therapy. So you suggested in the past that there is a physiological cause for schizophrenia, that it’s not just, quote “all in the patient’s head.” What exactly do you mean by that?
Albert Mensah: You know, we’ve had this misconception. We’ve had a mis-analysis that goes back to what I would call psychiatric antiquity. We look at schizophrenia and conditions like bipolar as though they’re mental health phenomena. And they’re actually not mental health phenomena. So what do I mean by that?
So, in medicine, the way psychiatry came about was that we would define every single test we know how to perform for the human body, for chemistries, for blood, for urine analyses. And when we found nothing and someone was behaving erratically or differently, we would then say, ah, this is a psychiatric disorder.
Okay. But what happens when you now test and find imbalances that correlate with the strange or average behavior of the patient? By definition, it’s no longer a psychiatric disorder. It’s now a medical disorder, an actual medicine phenomenon, meaning we have symptoms, we have a history, we have testing that reveals the underlying mechanisms or disorder, and then we have correction or at least improvement. By definition, that’s a medical problem, not a psychiatric problem. So when we were talking about physical or physiologic issues, we’re talking about the very dysregulated factors that go into the production of the symptoms that lead to a diagnosis of schizophrenia.
So in other words, when you say “it’s in your head,” well, guess what? It may be in your brain, but it may not be part of your actual mentation. When we talk about physiology or physical, it may actually be in your body. For example, approximately 6% of individuals who come down with a diagnosis of schizophrenia actually have as a cause an inflammatory bowel disorder. Guess what? Treat the inflammatory bowel disorder in these people and the schizophrenic signs and symptoms go away. By definition, did they ever have schizophrenia? No. They had an inflamed bowel, oftentimes due to dietary infractions and dietary inflammation in the system. And that’s why they began to behave the way they did.
So we’ve become a lot more savvy about what is really causing what, in the world of mental health. And we’re finding that a lot of mental health is not mental at all. It’s actually physical or physiologic.
David Stouder: Well, that’s interesting because, I mean, I would get the impression that most practitioners, if I came in acting, you know, like I had schizophrenia, erratically, and they said, oh, his gut is messed up or inflamed, they would say, well, that’s something different, let’s move on. So what you’re saying is we need to look… There are a lot more things in the body, to use maybe a cliche term, holistic. But if we look at these patterns, it may not be just something is all wrong in your mind. There’s actually a physiological…
Now, are you on the cutting edge of this? Are many practitioners using this approach or is this something you’re developing?
Albert Mensah: No, absolutely, we are. It’s not even in development. Here’s the funny thing. This was developed a long time ago by the fabulous Dr. Carl Pfeiffer. I call him sort of the grandfather of our process here, generationally speaking. He was the one, MD, PhD, who got tired of what we see in traditional psychiatry, seeing patients, you know, snowed with medication and said, there’s got to be a cause for this. And he evaluated these things and found these imbalances. And guess what? People woke up from catatonia. People normalized their lives from schizophrenia and bipolar disorder and no longer had a diagnosis, all by correcting the biochemical imbalances that were in the body and in the brain.
So this is not new. This is not Mensah doing this. I’m honored to have been part of the process of the education, and therefore we teach globally, we speak globally about this because we have to educate people and let them know, wait a minute – this is not some mystical phenomenon that has to do with the time your dog died 50 years ago. Or the problem you have with your mother or whomever, or whatever relationship.
This is about biochemical aberrations. It’s oftentimes a combination of what is an environmental insult, superimposed upon genetic predisposition. So we do have a combination of environmental factors, but superimposed upon an internal dysregulation or weakness. That’s what we call epigenetics. Now THERE is the field for today: epigenetics, how the outside world affects us.
David Stouder: Right. In other words, how we have genes, but they… there’s input from the environment, our inner and outer environment, that causes them to express.
Well, this brings me to another question. I mean, my impression, and I don’t know if this impression is just from, you know, with social media connecting you to everything everywhere, but it seems like cases of schizophrenia and some of these similar kinds of disorders are on the rise. One is, do you agree? And if so, do you have an idea of why that would be?
Albert Mensah: Absolutely. First of all, I do agree. And let’s look at the world we’re in right now. If we talk about the development of schizophrenia or bipolar disorder, either one, as being related to some type of stress-induced insult or phenomena, let’s look at the world we’re living in currently. We have a global pandemic. We have people sequestered from their families. We have relationships in challenge. We’ve got internal stressors, external stressors, we’ve got emotional dysregulation, we’ve got business variables. People have lost their jobs, are losing their homes. What part of stress isn’t happening in the world today?
Are we surprised then that individuals who may have a genetic predisposition, when we now superimpose an outside stressor, that we’re showing up and seeing more schizophrenia? And let me say something also that’s oftentimes controversial, but it really isn’t. It’s more about financial compensation. But now the legalization in many states of illicit substances like marijuana – this is not a question, it is fact. One in six males who even uses marijuana periodically will develop psychosis or schizophrenia. I treat these individuals. I see it all the time. We said this before it was legalized. We certainly talked about it when it was in the process of legalization in the state of Illinois, and we spoke against it.
So let’s take all these variables now. We’ve got illicit drugs. We’ve got outside stressors and influences. We’ve got a world in global chaos. Yes, we’re going to see more of these so-called diagnoses labeled schizophrenia.
Now I want to be very clear. Schizophrenia is not one disease or disorder. It is actually a family, a group, a constellation of syndromes that have similar patterns and therefore they’re labeled as one disorder. They’re not. Okay. It is not. Schizophrenia is a group of different chemistries, different situations that lead to dysregulated mental processing and therefore behavior.
David Stouder: So, you know, I’ll look at it this way. Obviously, medications can provide some relief, they play a role in all of this, but I think we’re moving… I think what you’re going to say here is that yes, some of these traditional drugs have their uses, but we need to go beyond that because just covering up, tapping down some of the expressions of the problem are not getting to the root cause.
Albert Mensah: Absolutely correct. Absolutely. And please don’t misunderstand me. I’m not actually even saying in this instance that these medications are bad. No one is speaking against the medication. Many times individuals need to have some level of immediate temperance or quick temperance of symptoms in order to try to gain some level of stability, whether it’s emotional or physical, or even just functional stability. But they’re not getting to the root cause of the issue, and that’s where you need to have a good biochemical assessment in order to determine where the dysregulations are and then look to correct them. So yes, medications can be useful, but they’re not the key treatment. They are a temporizing measure. Absolutely.
David Stouder: Well, you had mentioned in the beginning that people expressing schizophrenic symptoms, and then it turned out in this case you mentioned, to be like gut inflammation, and when the gut inflammation was corrected, the symptoms went away. Unlike medications, then you become dependent on them. The symptoms can go away when you’re taking them but, you know, they all have some downsides, so if we could minimize or not use them in certain cases, I think that would be, obviously, to everyone’s benefit.
Albert Mensah: Without question. Absolutely. I will state though that, and this is odd for me to say, but in defense of the pharmaceutical industry here for a moment, many of these medications in the short term are not quite as problematic, outside of their side effect profile. It’s when folks are on these things for years and years and years, and we start to see more challenge with regard to the difficulty of either weaning off, or how our patient is actually able to recover from their original condition because of the medications. But sometimes they’re just very necessary short-term pieces.
David Stouder: I think you make a lot of sense there. And before we end up, I do have a question, before we give out your website. So you’re in Illinois. People hearing this interview that are interested in what you’re saying, and maybe not getting this kind of approach around here or where they are. Are you able to work with people remotely?
Albert Mensah: Oh, absolutely. COVID has forced a lot of change in the field of medicine. So now with telemedicine and telehealth, our patients are more easily accessible, literally globally. So we have patients from all over the country and literally different countries on the planet. So it’s a great opportunity to learn about different cultures, to meet different people, and to be able to provide some level of service.
David Stouder: Dr Mensah, thank you. I think that’s going to mean a lot to a lot of people. Now, we want you to know that Dr. Mensah can be found at www – and I will spell it – MensahMedical.com, and that’s M-E-N-S-A-H-Medical.com. And I’ll remind you to subscribe and get all the Humanized videos, podcasts and transcriptions from all of our thought leaders on personalized health at HumanizedHealth.com. Dr. Mensah, thank you again.
Albert Mensah: Thank you very much.








