The Impact of Trauma on Brain Health
Featuring
Aimie Apigian, MD, MS, MPH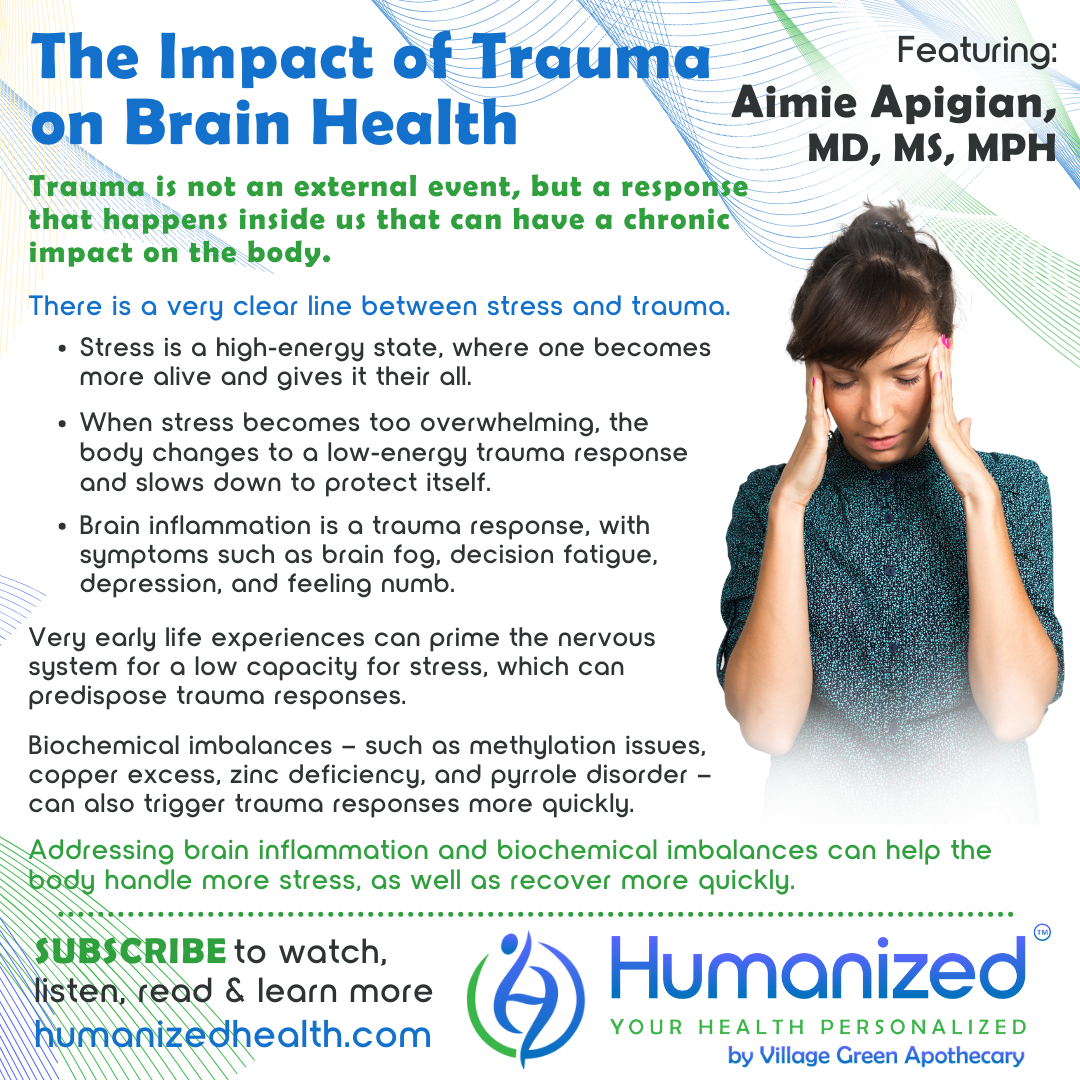
WATCH
LISTEN
READ
Rebekah Kelley: Welcome to the Humanized Podcast, all about personalizing your health. I’m your host, Rebekah Kelley, and today our topic will be The Impact of Trauma on Brain Health, with Dr. Aimie Apigian. Before I introduce Dr. Aimie, I want to remind you to go ahead and subscribe so that you can get all of the variety of casts in audio, video and transcription at HumanizedHealth.com. And I’d also like to thank our lead sponsor, Village Green Apothecary, at MyVillageGreen.com.
A little bit about Dr. Aimie. She’s a double board certified medical physician in both preventative and addiction medicine. She holds a double master’s degree in biochemistry and in public health. She’s a leading medical expert on addressing stored trauma in the body through her signature model and methodology, The Biology of Trauma™, a new lens that courageously up-levels the old method of trauma work in medicine by reverse engineering trauma’s effects on the nervous system and body on a cellular level. Dr. Aimie specializes in trauma, attachment and addictions after having personal experience in foster parenting, adopting, and then having her own health issues that were a result of childhood and life experiences. In addition to her medical studies that have included functional medicine certification, she has sought out trauma therapy training since 2015. A three-time summit host, Dr. Aimie founded a non-profit called Family Challenge Camps and developed and ran weekend intensives for families with children who have experienced attachment trauma. She is currently the founder and CEO of Trauma Healing Accelerated, where she bridges the two worlds of functional medicine and trauma therapy with a mission to help adults accelerate the healing journey by addressing the biology of trauma that keeps stored trauma stuck in the body, mind and spirit. Her provider certification course teaches providers to do the same for their clients.
I just want to say, Dr. Aimie, it’s wonderful to have you back. Thank you so much for coming.
Aimie Apigian: Thank you, Rebekah. I’ve been looking forward to this.
Rebekah Kelley: Me, too. So, I just want to hear all about it. I remember in our last session you kind of teased us with such interesting perspective and so I’m so glad you’re back here. And I just want to ask you, how can trauma cause permanent changes in one’s nervous system?
Aimie Apigian: Ooh, that’s a great question and it leads me to the common misunderstanding of trauma. And so many people think of trauma as being an event, and it was that thing, or it was that thing, or I don’t have trauma because I don’t have that event. And when we look at actually what trauma is, and when I started having to understand it on a physiological level, I saw that no, that trauma actually is not an event at all. It’s not anything external to us, in fact. It’s everything that happens inside of us in response to our environment. And so when we see that, we see that there’s this very clear line between what is a stress and what is a trauma.
In medicine, we have this term that’s called homeostasis, which is basically your body’s ability to keep your physiology within this window of health. Like, alive, right? Not necessarily optimal health, but hey, we’re getting through, we’re managing things. And what trauma is, is the body’s measurement of its physiology in that moment. And it says, ooh, I think that this stress is too big for us. I don’t think we’re going to make it, and I think it’s going to disrupt our ability to maintain homeostasis, threatening our survival, and so I need to shut things down.
Stress is different, Rebekah, because a stress is something where you get actually more alive with it and you can sense that, ooh, this is a lot and I wonder how this is going to turn out, but I’m going to give it my all. That is still a stress, where it’s a very high-energy state. The minute that that stress to your body is overwhelming, your body changes into a low-energy state. In fact, it’s conserving energy because homeostasis has been threatened, and it does this to protect us, no matter what the cost. And the cost is a big cost, because the cost is downstream effects on our biology that don’t go away. But it’s willing to pay that price to save us in the moment. The problem is, is that when some of us have had very early life experiences that programmed our body to respond this way to stress, now with even the smallest amount of stress, it overwhelms our physiology. And so we notice that our capacity for stress is really small. We think that we should be able to manage more stress in our life without it taking us down, without it overwhelming us. And it’s likely true, we should be able to handle more stress. But for many of us, these patterns have been in our nervous system, in our wiring, since early life. And at the first hint of a stress or a threat, our body’s like, nope, nope, I’ve already learned that I’m not big enough, I’m not strong enough to handle stress, so I should just immediately go into the trauma response, which is this low-energy state, and with all of the downstream effects to our biology that don’t go away like they do with a stress response.
Rebekah Kelley: So every time you describe things, my mind has to rethink how I think of things. Does that make sense?
Aimie Apigian: I love that, Rebekah. And I love that I can do that for you [laughs].
Rebekah Kelley: I’m taking this in and I’m like, what you’re saying makes so much sense to me, but I’m having to recalibrate kind of how I think of trauma, right?
Aimie Apigian: Yes. And that’s everybody, Rebekah. We have misunderstood trauma completely. And so it really is this whole redefining of trauma if we’re going to understand the chronic effects of trauma on the body.
Rebekah Kelley: So in terms then of our brain health, mental health, you’re saying that the body’s kind of recalibrating itself, right? Because of the situation that it’s in. What’s happening? What are those common biochemical imbalances that are resulting from this experience?
Aimie Apigian: Yeah, so one of the first things that I noticed, because of course this all came out of, first of all, my personal experience, right? And what I noticed happening was that when I would go to that shut-down place, life had become too much, and I would feel my body now going into that collapse, that draining of energy. Now all of a sudden everything feels heavy. It takes a little bit of training for you to recognize when your body goes to that place, if you’re not used to tracking your system. And once I started noticing when it went to that place, I noticed what happened to my mind. And it was consistent. When I would feel my body going into that trauma response, within hours I would get the brain fog, I would get the decision fatigue, I would get the everything is just hard. Of course, you feel a little down, but it’s also, you just kind of feel numb. And I thought, how interesting. And I started tracking that and sure enough, every single time my body went into the trauma response, my brain would follow with its own trauma response, I guess you could call it. And so that’s when I first started leaning into understanding brain and this brain inflammation piece first of all. And what I discovered was that part of the trauma response is this inflammation response in the brain. And the reason for that is because the trauma response is such an energy conservation response, that of course, it’s going to shut down the organ that uses so much of our energy, which is our brain, our mind. It’s going to shut that down. And we have these cells in the brain called glial cells or microglial cells, and these cells protect our neurons, which are the actual nerve cells in our brain. They protect them, they’re the guardian. Sometimes people refer to them as the gardeners who tend them, who prune them, who water them, who feed them, who clear out the debris. And so they’re amazing and they actually control so much of what happens in our mind, or our brain, and can become primed. And when they become primed, now with other things, stressors – and I’m going to use that term very loosely right now, and then I’ll come back to that – stressors will reactivate primed microglia. And that is exactly what happens when the body goes into the trauma response. That trauma response becomes a reason, a stressor that reactivates primed microglia.
Now it is possible that a person has had an event in their life that caused such a severe trauma response in their body that it was the reason for the initial priming. But sometimes it can be that we hit our head, we had some type of whiplash, maybe even a concussion, maybe we played sports. There are many reasons why a priming event will happen, but once we have some microglia that are primed, when our body goes into that trauma response, it’s an automatic trigger to reactivate those primed microglia, and we experience the brain fog, the decision fatigue, some depression. Not as much anxiety as before the trauma response because again, we just kind of feel numb at this point and just going through the motions until our body comes out of that trauma response.
So that was one really crucial piece that I was able to learn about for my own system. And then I started to see, wait a second, this is just the trauma response in everybody. This is what the human body does to protect itself. It has to shut down those organs that are consuming the most amount of energy.
So then you mention the biochemical imbalances, and that’s what has been really fascinating and a really important piece too, with this understanding the trauma response and triggers for the trauma response. There are, what I’ve identified as three most common biochemical imbalances that actually predispose us to going into a trauma response in response to a stress. That would be methylation imbalances, which if you understand anything around the neurotransmitters and methylation, you would know that undermethylators specifically, often, not always, but often have lower activities of serotonin and dopamine. Lower activities of serotonin and dopamine are really going to affect your early attachment and neurodevelopment. So that’s going to predispose you, because now you’re going to have had early life experiences where you went into that freeze response or the trauma response, because everything is overwhelming as an infant if you have low serotonin and dopamine activity.
But even as an adult, life is just harder if you feel that you’re down and discouraged and you don’t have that dopamine, you don’t have that serotonin. And so you’re going to be going into that trauma response earlier than someone who has their methylation cycle fully supported or didn’t have methylation imbalances to begin with.
The other ones that I see are the copper imbalances, so copper excess, zinc deficiency. Dr. Walsh specifically talks about how zinc deficiency is one of the most common nutritional deficiencies in all of mental health. Well, a lot of mental health, when you look at it through this new lens of trauma and stress, Rebekah, a lot of mental health is this going into the trauma response. And that zinc deficiency makes your nervous system so much more reactive, so much more sensitive, that again, the smaller stressors overwhelm your system and your system is going into the trauma response.
Same thing with a copper excess. Not only is the copper excess irritating your nervous system, but it’s also causing an excess of adrenaline to be released. Wow! Okay. So now you have even higher amounts of adrenaline with the stress response. That adrenaline, what does it do? It makes your heart race. It makes your lungs breathe faster, and that can disrupt homeostasis if it gets out of control.
And so if your body is sensing, whoa, whoa, whoa, whoa, whoa, we’ve got too much adrenaline, it’s going to initiate, trigger, that trauma response in order to save you, even though it comes at a later cost. So the copper excess and zinc deficiency often go together, so I lump those together.
And then the pyroluria, or the pyrrole disorder. Again, that causes a functional deficiency in zinc and B6, both of which are super important for the stabilization of the nervous system, but then also cause neurotransmitter imbalances. So you’re low in dopamine, you’re low in serotonin, and you’re low in GABA.
So your whole brain is crucial and central to this trauma response in the body, both causing it, predisposing you to that trauma response, but also then especially with that brain inflammation piece, being a result of the trauma response.
Rebekah Kelley: Wow. I always am just in awe of the body and how it tries to balance itself out, right? And so you’re basically sharing what’s happening on such a physiological level, right? All the little chemical firings that are happening and what your body’s doing just to manage that, with everything else going on. And it’s such a beautiful way to explain it, because sometimes it’s so easy to be like, well, I’ve just got to get my butt off of this sofa and go do something. Right? But you’re dealing with so many other things, that it’s so hard.
So with all this description and all this happening, can you tell us a little bit about how can you help people heal and rewire the brain, if this is what’s happening, if this cascade is what’s going on? What’s that process?
Aimie Apigian: Ah, there’s so much hope, Rebekah, because we have the tools to support your microglial cells with that inflammation, and so we can actually help them recover faster and your body can then come out of the trauma response faster. Then if we support those microglial, sometimes we can even help you hang with a stress and not go into the trauma response because we’re supporting your brain inflammation and those primed microglial cells. Even with the biochemical imbalances, when we can support them, when we can bring in the zinc so that you don’t have these functional deficiencies, we can support the nervous system and now it can hold more stress.
And so you actually are seeing huge changes in people when you can come in and support their body. And like you say, the body is a beautiful thing. It is doing its best. And when we help it perform at its best, specifically, being able to target those things that really take it down and predispose it to the trauma response, the changes to people’s lives are incredible. Incredible. It’s so wonderful to see, very meaningful to see them being able to change things about themselves that they just never thought that they’d be able to change. They just thought that this was who they were and their personality, and it’s actually not.
Rebekah Kelley: And they thought they were stuck, I’m sure, right? They thought they were stuck where they were. And you’ve discovered a way to kind of help get them out by providing the support that they need.
Thanks so much, Dr. Aimie. As always, you blow my mind. Dr. Aimie can be found at www.TraumaHealingAccelerated.com. I’m just going to spell that. T R A U M A H E A L I N G A C C L E R A T E D.com. Let me remind you to subscribe and get access to all our Humanized videos, podcasts and transcriptions from all of our thought leaders like Dr. Aimie on personalized health at HumanizedHealth.com.
Please come back and visit us again. It’s always a pleasure.









