The Importance of Microglial Cells in Mental Health
Featuring
Brendan Vermeire, FDN, CPT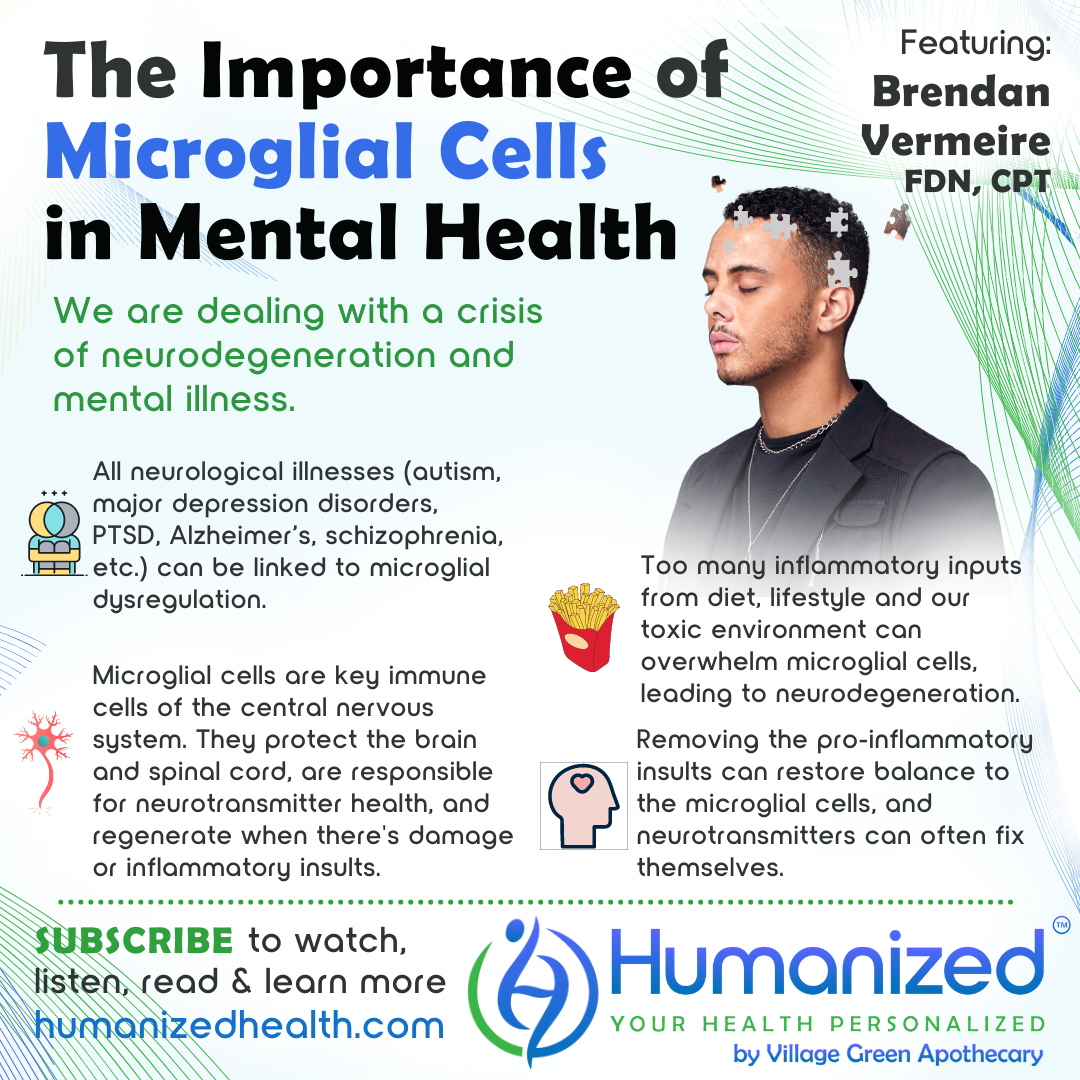
WATCH
LISTEN
READ
Rebekah Kelley: Welcome to the Humanized podcast, all about personalizing your health. I am your host, Rebekah Kelley, and today we will be discussing Microglial Activation and Mental Health Dysfunction with Brendan Vermeire. And Brendan, thanks for being here with us.
Brendan Vermeire: Thanks for having me, Rebekah. I always have a lot of fun with these types of conversations and podcasts. That’s really what I live for, so it’s really a pleasure to be here with you.
Rebekah Kelley: Awesome. So anyway, before we get right into it, I want to remind everyone to subscribe and get all of the other variety of casts in audio, video and transcription at HumanizedHealth.com. I’d also like to thank our lead sponsor, Village Green Apothecary, at MyVillageGreen.com.
Now a little bit about Brendan. He’s a functional medicine consultant, clinical researcher, board certified holistic health practitioner, master nutrition coach, master personal trainer, USAW Sports Performance Coach, and CrossFit Certified Trainer. Brendan is regarded as one of the top leading experts in metabolic health and holistic education. He is the proud owner of the Metabolic Solutions Institute, dedicated to educating health professionals and clinicians with cutting edge strategies to best serve their clients and patients.
So excited to talk about it. So, Brendan, what are microglial cells?
Brendan Vermeire: Yeah. Well, thanks for that flattering bio. I never get used to hearing it read back to me and everything. And it’s like, oh, I guess I have done a lot.
Rebekah Kelley: You have, yes you have.
Brendan Vermeire: And so it’s been interesting to, having started as a personal trainer and nutritionist to then be here where most of my life now centers around clinical research, specifically around the subject of microglial activation, which is so specific and so kind of niche down. But it’s been a beautiful journey to get here in a very kind of organic evolution as my interests and curiosities have developed.
So with microglial cells, getting right into it, microglia are the innate immune cells of the central nervous system, so thinking about white blood cells of the immune system that are there to protect us and remodel tissues and clean up debris and all of the amazing things that we love the immune system for.
And so in the central nervous system, we have all different types of glial cells. We have astrocytes and microglia and macroglia, and all these different things. And microglia, I really describe them as the guardians and the architects of the central nervous system. They are exclusive to the central nervous system. So brain, spinal cord, on the other side, the blood-brain barrier, they are exclusive to that part of the body. And researchers, scientists, they used to think that the microglial cells were actually macrophages from the periphery that had migrated into the parenchyma and the tissue of the central nervous system, but then they figured out, actually, these are two different cell types with two different cell lineages, but they were very, very, very similar.
So all of the audience that might be familiar with monocytes and macrophages, these are basically the monocytes, the macrophage of the central nervous system. So that’s where I think the architect and guardian is a perfect analogy because these microglial cells, their job is, they are the first line of defense in the brain. So if we have any sort of pathogen or inflammatory insult or damage like a concussion or something, they are the first line of defense to use inflammation as the “cleansing fire” to burn off the debris or fight off the pathogen, or whatever it is. But also they’re the architects in the sense that they co-regulate neuroplasticity and neurogenesis, which is really just fancy words for saying the remodeling of the neural connections of the brain. So we have tons and tons of these neurons, and we’re constantly producing new neurons, new brain cells, which is antagonistic to the previous belief, which was [that] you’re born with so many brain cells, you don’t get more.
Rebekah Kelley: Yeah, don’t burn them out, they would say. Don’t burn them out.
Brendan Vermeire: Exactly. They used to think that our neural networks were very stagnant and non-malleable. And so that’s where, with neurodegeneration, which has become the sixth leading cause of death in the United States, now researchers are starting to think about Alzheimer’s as like a type three diabetes. There’s a lot to unpack there, but the neurodegeneration aspect has really driven, like, we need to figure out why does the brain degenerate? And really it comes down to these microglial cells and their activation.
So there’s a lot to unpack with what drives microglial activation and what causes a dysfunction. Because under normal, healthy, physiological circumstances, these microglial cells appropriately fight off the foreign invader, repair the damage and regenerate the brain.
So if we’re dealing with a crisis of neurodegeneration and mental illness, these cells have become the focal point of psychiatric research and neurodegenerative research. And this is where I’ve really kind of dedicated my whole career, to unraveling these things. Because big pharma, they’re already working on some fancy drugs that are targeting different proteins and receptors on the microglia. So they recognize, if we can create drugs to modulate the activity of these cells, we’re going to create the next billion dollar drug. So as consumers, patients, clients, practitioners, professionals, we need to catch up on that science so that we can functionally use the same science and holistically, naturally use that to repair our own brain, so that way we don’t become excessively reliant on the next pharmaceutical drugs.
Rebekah Kelley: Right. That’s a beautiful description. I love how you explain what a microglial cell is because I’ve heard it, but I don’t fully understand it. So considering how you just described it, what does microglial dysfunction look like? What are those symptoms? I mean, you’ve named a few things, but what does that look like? An activation syndrome? What does that look like?
Brendan Vermeire: So, some of these pseudo-diagnosis things that we talk about in the functional medicine space, I think they could be helpful or hurtful depending on how we communicate them. Right? So, leaky gut, leaky brain, mitochondrial dysfunction, and mass cell activation syndrome has gotten really, really popular. So I will admit – I’m not a hypocrite – I was inspired by the mass cell activation thing. I was like, well, if we’re going to get all hot and bothered and crazy about mass cell activation, I think microglial activation is just as important, if not more important.
Now ultimately, it’s just a phrase, but I think understanding what that is and understanding the role of microglial cells in mental illness and neurodegeneration. So I hope people use my terminology appropriately because we do have to keep in mind, immune cells, by evolution, by nature, they are designed to be activated. That’s the whole point, right? So we could easily say there’s a platelet activation, an eosinophil activation syndrome, but with that sort of disclaimer and retort expressed, microglial dysregulation is really what leads to mental illness and neurodegeneration. Like, all across the board. I mean, we’re talking autism dysfunction and just lower functioning autism, schizophrenia, major depressive disorder, PTSD, Alzheimer’s, Parkinson’s, ALS, multiple sclerosis – like literally every single neurological illness can very much be linked back to microglial dysregulation.
So this is where I’ve created courses and stuff around this for providers. And understanding this core concept of, under normal, healthy physiological circumstances, these microglial cells are inactivated. Which actually, I think that’s misleading. They’re quiescent, which is not the same thing as inactive. They’re just patrolling the environment. So if you think about a police officer that’s just doing his rounds around the city, making sure everything’s calm and under control, he’s just chilling and cruising. So that’s quiescent, which is usually said “inactivated,” but they’re patrolling. But then what happens when the police officer gets, you know, radio signals, like there’s a bad guy that you got to go arrest or shoot or whatever, he’s going to turn his sirens on, stomp on the gas pedal, and he’s going in full-blown GI Joe mode.
So that’s going to happen with these microglial cells when they detect some sort of danger or threat. That could be some sort of pathogen or an antigen or inflammatory insult or toxin or whatever it is, but they need to become activated into… They have two primary phenotypes. So you’ve got these quiescent microglial cells. And then when they’re becoming activated, they’re either going to morph through what’s called microgliosis, just the morphology as they change their form, they actually get kind of big and bulky and puffy, whereas under their normal quiescent, they’re kind of like an octopus, they’re kind of small with these long arms, but they beef up a lot when they go GI Joe mode. And in the M1 phenotype, this is your cytotoxic, pro-inflammatory, neuro-destructive GI Joe, ready to kick down doors and shoot bad guys – that’s what that one is. But then you have this M2 phenotype, which looks structurally very similar, but this is neuroprotective, neuro-regenerative, anti-inflammatory.
And so ultimately, what we actually have seen through the literature through measuring different surface protein markers that you can only do in clinical research, Petri dish kind of technology… but they’ve seen that it’s not really one or the other. It’s not like these cells, they turn into M1 neuro-destructive, versus M2 neurogenerative. They can actually be a little bit of both. They’re highly dynamic so they can actually be shooting and spitting out pro-inflammatory cytokines, but they can also be releasing neurotrophic factors and anti-inflammatory cytokines at the same time.
But this is why I call them the guardians and the architects, because it’s kind of like a firefighter, GI Joe, policeman, all in one. They’re not a one trick pony. And so basically it’s more of a spectrum of activation. And they can be doing different things in different brain regions, right? Just because you have a lot of M1 phenotype in your hypothalamus doesn’t mean that your frontal lobe is pro-inflammatory. There’s something else going on over there.
There’s millions of these microglial cells in the brain. They make up about 10% of the cell population in the brain. So they’re greatly outnumbered by other brain cell types, which is why they’re so critical. They’re kind of like the Marines or the special forces. Really though, we have to be looking at the net effect of how much is the scale tipped towards the M1 neurodegenerative, pro-inflammatory phenotype. And that’s what most Americans, like literally the whole American population, is dealing with because of the standard American diet, lifestyle, toxic environment, so on and so forth. Our brains are quite literally, and our microglial cells are quite literally overwhelmed with all of these pro-inflammatory input signals. This is what leads to neurodegeneration, is then there’s too much nerve destruction, too many pro-inflammatory insults, and what we need is to tip the scales back to homeostasis, where there’s a balance of M1 and M2. So most people with the standard American brain, standard American mind, they’re heavily skewed towards that M1 phenotype.
Rebekah Kelley: I love how you also… you know, I love Marvel comics. So give me this visual of these fighters coming in to deal with, as it relates to what the body needs.
So, can you then explain how microglial dysfunction and, I mean, you’ve touched on it, but how does that relate to mental illness and mental health? I guess mental wellness maybe is a better way of saying it, but how does that connect?
Brendan Vermeire: Sure. I mean, certainly mental health can be multifaceted. Is it more psychological, emotional, kind of stress driven, or is it more of a physiological dysfunction that’s then causing symptoms of mental illness? So it can be very ambiguous and multifaceted.
But in regard to mental illness, the classic narrative is mental illness is driven by these neurotransmitter brain chemical imbalances, which is based on a theory that’s like 40 years old. And we have decades of new research that lucidates, well, yes, neurotransmitter imbalances are part of what’s going on there. But we now really see that inflammation is upstream from that. So there’s actually two key pathways, both of which are biochemical pathways expressed in microglial cells, where under the presence of heightened inflammation, oxidative stress, it totally disregulates our neurotransmitters because these key pathways, these key GTPCH1 and IDO1, and these two key enzymes that actually go to contribute to producing serotonin and dopamine and GABA and glutamate and all of our kind of primary neurotransmitters, those get totally dysregulated when these microglial cells are activated into their pro-inflammatory state. So in a lot of ways, with mental illness, if we remove the pro-inflammatory insult, if we can restore balance to these microglial cells, the neurotransmitters will kind of fix themselves. But most of our therapeutics and drugs and psychiatric care and model is based on working on the downstream neurotransmitter imbalances, and they’re not really doing anything about the upstream microglial dysregulation.
Rebekah Kelley: Wow. Thanks Brendan. Those are really valuable insights. Brendan Vermeire can be found at Brendan@MetabolicSolutionsLLC.com. And let me remind you to subscribe and get access to all Humanized Health videos, podcasts and transcriptions from all of our thought leaders on personalized health at HumanizedhHealth.com. Thank you so much, Brendan. It’s always very illuminating to talk to you.
Brendan Vermeire: Thank you, Rebekah. It was great.









