When It Comes to Bowel Movements, What is Considered Normal?
Featuring
Julie Ann Davey, RN, MSN, ANP-C, ACNP-C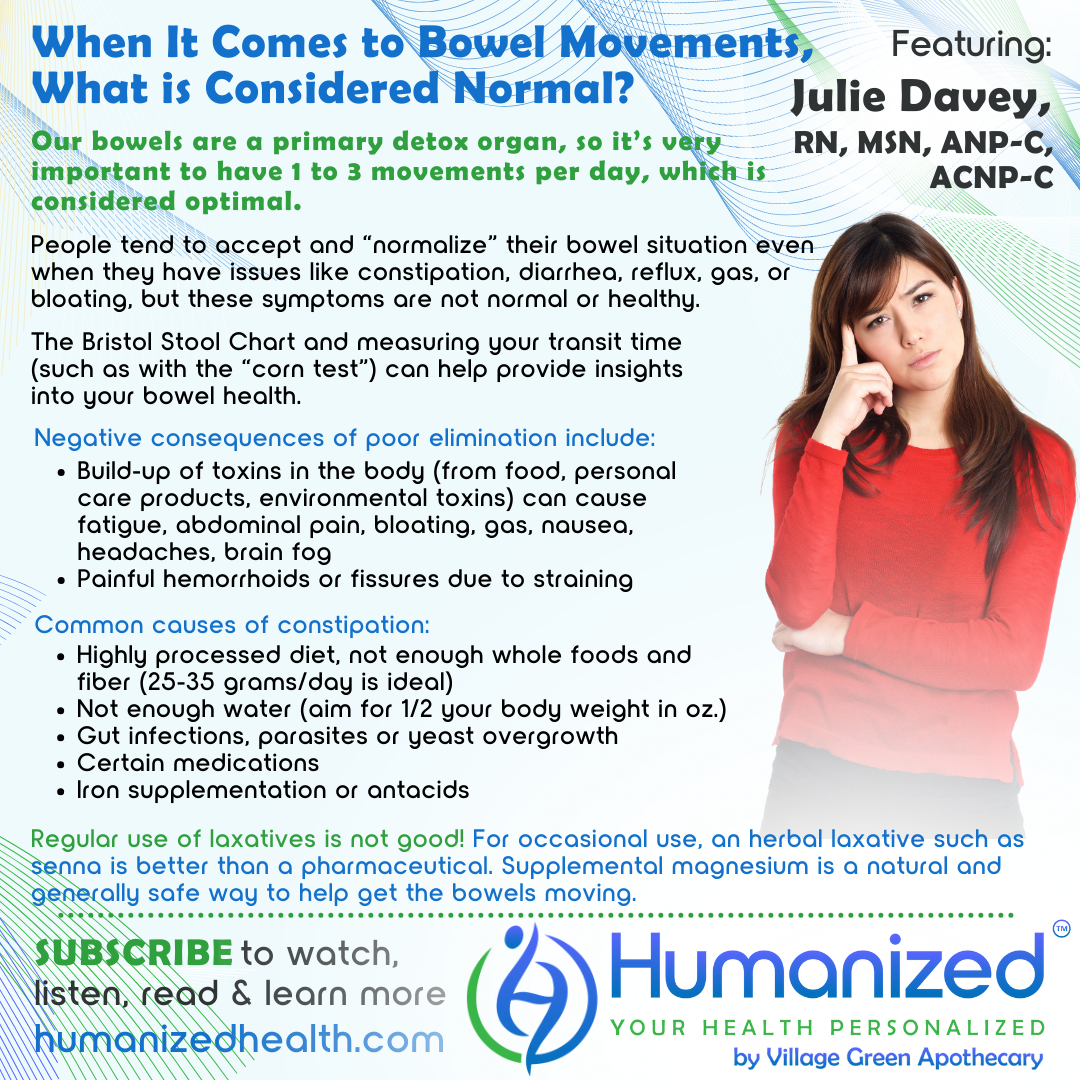
WATCH
LISTEN
READ
David Stouder: Welcome to the Humanized podcast. This is all about personalizing your health. I’m your host, filling in for Rebekah Kelley. I’m Dave Stouder. Now, I’m really excited about this topic today because I talk to a lot of people in Village Green Apothecary, and we talk about digestion, we talk about elimination. And when we talk about elimination, and I ask people if they’re regular, their answers are all over the map. So, we will be discussing, When It Comes to Bowel Movements, What is Considered Normal, with our frequent guest, nurse practitioner Julie Davey. Now, before I introduce Julie, I want to remind you, you can go on MyVillageGreen.com and for free, you can access all of these podcasts. You can watch the video, just listen to the audio, and also download transcripts. So it’s a great free service, and we thank Village Green Apothecary for that.
Now, Julie Davey is a nurse practitioner with over 25 years of experience. She’s passionate about educating others on the power of food and natural medicine to heal the body. Her clinical practice primarily focuses on GI health, where she utilizes specialty lab testing to help clients get to the root cause of their symptoms. She creates tailored protocols and empowers individuals with the necessary tools to live a healthy and vibrant life. And don’t worry, we will tell you how to get in touch with Julie after this interview concludes.
Julie, welcome back. We’re so glad to have you.
Julie Davey: Thanks, Dave. I’m excited to be here. What we’re going to talk about today I think is such a huge issue for so many people. So I’m excited just to dive into the discussion.
David Stouder: Well, I’ve noticed when I talk to people, they’ll say “my digestion is slow” – and to me, I think of digestion as breaking down nutrients and then elimination as having bowel movements, in terms of we’re going to talk about the bowel. And a lot of people, I guess, out of politeness, say “my digestion is slow,” and that means they’re not eliminating well. Now I talk to people, they go once a week, they go every other day or so, they go three or four times a day, and everybody I think just accepts what they have, unless it’s a really bad problem. So I know everyone’s individual, but how would you define, I mean, what is considered normal when it comes to bowel movements?
Julie Davey: Yeah, I think that’s a great place to start. So, our digestion and elimination, our bowels are one of the primary detox organs. So, really, really important that we work on getting to a normal state, let’s say. And if we’re looking at what is normal, as you said, I mean, there’s a lot of bio-individuality, right? We’re all a little bit different. But generally, one to three regular bowel movements a day is what’s considered normal. Now we’re talking formed, soft, no straining, things like that. So that’s what we’re striving for.
And if anybody’s interested in what this should look like, I know this is kind of a topic that some people don’t want to… oh, I don’t want to look and see. But this is really important. This is a super important piece of your health. There’s actually a chart called the Bristol Stool Chart, and you can just literally Google it. It’s spelled B R I S T O L. If you just Google that, it will pull up images that will show you exactly what your bowel movements should look like.
But it should ideally be one to three times a day. Because if you think about it, when we’re putting food in, yes, we’re breaking it down, hopefully, and absorbing nutrients, but it’s got to go somewhere, right? It shouldn’t stay compacted in there. So if you think about how many times do we eat a day, you should be eliminating, maybe not necessarily every time after you eat, but at least one to three times a day.
David Stouder: Well, that’s good. Now, let me run something by you that I think I read once and it sounded like it makes sense, but I’ll run this by you.
So like you said, they said to be regular, you ought to be going one to three times a day. And they said, if you only go once a day, it’s probably optimal to move about two feet of your bowels. So, if you only go once a day, it should not be a small bowel movement. And then the third thing I was told was that there’s also, you might go once a day, but if what you eat on Monday comes out on Thursday, that’s not good, so they suggested the corn test. Eat some corn kernels, and if you eat it on Monday, it’d be good to see it within 24 hours. Does that make sense?
Julie Davey: Absolutely. Yes, there are several different things that you can do to really test that out. Corn is one of them and that’s probably one of the best ones because it’s an easy visual. There are other things, like you can consume beets and look for the color change, things like that. But yeah, you want to ideally, what you’re eating, if you are seeing that come out in the stool, you want to see that within 24 hours. You don’t want to eat corn and then see it 3 days later. That’s not good. So yeah, I think that’s an easy way. If you’re questioning, is my digestion slow and, really, you should know if you’re not having one to three bowel movements a day. But if that’s something you wanted to test out, then certainly you could do, like you said, the corn test. That’s an easy way to kind of figure that out.
David Stouder: Now, so many of us, especially with digestive issues, even like, constipation, diarrhea, reflux, and bloating, a lot of times we just adapt and accept. Oh, I got some bloating, it’s all right. I don’t worry about it. I’ve got gas, well, it’s okay.
What are some of the consequences that… people are listening to us and they’re not regular by our sort of broad definition here that you established. What are the negative consequences of just saying, oh, I go once every 3 days, Julie. I’m okay with that.
Julie Davey: Yeah, I love that question because, the thing is, we do normalize things. Because I think what happens is, we get used to something. So then we say, well, this is normal for me. And it’s because you’ve normalized that for yourself. It doesn’t mean it’s actually normal and healthy. So if you’re not eliminating every day, then you are pretty full of toxins. Because think about the fact that our bowels, like I said, are one of our primary detox organs. We’ve got to be getting rid of these toxins that, a lot of times it’s things that we are putting into our body through food. It could be things that we’re putting on our body through personal care products, or even just environmental toxins. We’re exposed to toxins in a multitude of ways every single day. And if we are not, if our digestive system is not strong and we’re not eliminating properly, then these toxins are just kind of circulating and floating around in the body. And so, what could that cause? That’s going to cause you to have symptoms like fatigue, abdominal pain, maybe bloating, like you mentioned, gas, sometimes even nausea. Headaches is another thing that we see a lot of times with chronic constipation, and brain fog. So really, there’s this huge gut-brain connection, and so you can have a lot of neurological signs just from being constipated.
And then the other thing that you worry about too is, if someone has chronic constipation and the stool is really hard, and maybe they’re really straining to go, then you worry about things like hemorrhoids, or even fissures, where you get actual tears there in the tissue, and all of that is super painful, not anything that you want to experience.
So those are probably, I would say, the most common issues with not eliminating properly.
David Stouder: Yeah. And I think if, I mean, maybe we don’t want to think about this, but there’s all these toxins in the environment and plastics and xenoestrogens and things we worry about. And here we might just be having quite a bit of toxins sitting in our body that are supposed to be gone, and obviously these things get reabsorbed.
Now, I don’t want to leave this interview without talking about some of the natural solutions, but do we have an idea of what, again, thinking about bio-individuality, what causes constipation? Why are so many people, as I encounter them, constipated to some degree?
Julie Davey: Yeah. So let’s talk about the primary, probably number one cause is our diet. I mean, eating the standard American diet – highly processed foods, very little nutrition, very little fiber, which is key to having regular bowel movements. I mean, what we’re putting into our body is really kind of foundational and the first place you want to start. So if you’re eating a diet that, again, is not full of whole foods and grains and fiber, then you probably are going to have some issues with eliminating properly. So that’s one place that you can start and make some changes.
In terms of fiber, you do want to make sure that you’re getting enough fiber – 25 to 35 grams a day is ideal. And we ideally want to be getting that from whole foods, real foods, fruits, vegetables, legumes, things like that. Now you can add in some supplemental fiber like psyllium husk, or acacia fiber is another really great type of prebiotic fiber. That’s going to help you move the bowels, if you’re if you’re having enough fiber.
The other thing that goes hand-in-hand with fiber that we sometimes don’t do a great job on, is water. You’ve got to be having enough water to really kind of bulk up the stool. You want to be kind of striving for half your body weight in ounces a day. So, if you weigh 100 pounds, you’re striving for 50 ounces of water a day. And that’s an easy thing, to keep track of that. You’re going to feel so much better when you’re hydrated.
So lack of water, a highly processed diet. Those would be two big ones.
Other things to consider are, sometimes if you have certain gut infections, certain bacteria or parasites or yeast overgrowth, that can certainly slow the bowels down and cause constipation. So that’s something to consider, especially if you’re doing all of these foundational things and you’re still struggling. That’s when I would really suggest looking into some testing to see maybe if you do have a type of pathogen there that needs to be addressed.
But let’s talk about something that maybe people don’t even think about and aren’t told when they’re prescribed. Certain medications can certainly cause constipation. So, if you’re being prescribed things like narcotics, or maybe you have some type of chronic pain or even acute pain, after a surgery, let’s say, you’re having to take some narcotics, even for a week’s time. I see this all the time. That will 100 percent slow your bowels down and you’re going to really have to be doing things like I mentioned with diet and water to kind of counteract the effects of the narcotics.
Other things. Iron supplementation can cause constipation. Antacids. Any antacids that contain calcium like Maalox, for instance, or that contain aluminum, like Mylanta, those can slow the bowels down. Other medications that you might not know can cause some constipation are some antidepressants, especially things like amitriptyline, those cause constipation. And then a couple of our blood pressure medicines, calcium channel blockers that we use sometimes for blood pressure and also irregular heartbeats, things like verapamil and diltiazem. If anybody’s taking those and struggling with moving their bowels, that can be a side effect of those medications.
So, I would say, if you struggle with constipation, think about these things that I’ve mentioned, which are probably the top reasons, and see where you can make some modifications.
David Stouder: Excellent. And, one thing I want to point out, and this is one thing when we give out Julie Davey’s website you want to look into – the doctors, like you say, you can test for pathogens, parasites, but doctors don’t typically do this. Like when you go in and get a blood panel, you can say, oh, I got a blood panel and the doctor said everything looked great. Well, trust me, they’re not testing for that. So you might want to look into it.
Now, the other thing I just want to mention to everybody is that if you’re on one of these medications, and maybe you’ve been on it for 2 years and suddenly you have a constipation problem, just remember that these are adverse effects, not side effects. So a lot of times we take a medication and in the next couple or 3 months, they don’t affect us negatively. And then 6 months later, a year later… so, don’t discount, don’t say, well, it couldn’t be that medication, Julie, I’ve been taking it for 2 years. So look into this. We’re not saying throw away your medication, but we’re saying, be aware that it might be part of the issue.
Now, correct me if I’m wrong. Chemical laxatives and even herbal laxatives can be overused, right? They are best used for immediate results when that’s necessary. And so people, like you say, can hydrate, they can change their diet, they can add fiber. What do you think of people upping their magnesium a bit? Because I see a lot of people doing that to achieve regularity.
Julie Davey: Yes. So if you look at statistics and data, most people are deficient in magnesium. So it really doesn’t hurt in most all cases to add in some magnesium. That’s a great way to get the bowels moving. I like a product called Natural Calm. It’s just a powdered magnesium that you take. It’s great to take at night in a small amount of water because it’s very calming to the nervous system, so it could help with sleep. But yes, adding in some magnesium is a natural and generally safe way to help get the bowels moving.
And you don’t want to, as you said, Dave, you don’t want to become dependent on a laxative. That’s the last thing that you want. So if someone has to use something like that, more of a natural laxative like senna, something with senna in it, which is a plant extract, would be preferable over some of your more pharmaceutical type laxatives. But again, that’s temporary use, as you said.
David Stouder: Yeah, that’s true. And what I would say, I know that our guest, Julie Davey would agree, is when you get these signs from your digestive system, don’t ignore them. Things only get worse. And even if you’re constipated, maybe your bowel rhythm doesn’t get worse, but all these toxins are floating around in your body. And I think there’s a lot of people searching with their doctors and [looking for] medications for things, when they really just need to take some of your advice, Julie, with the diet and the fiber and make sure that they’re regular and eliminating. And so, I would just say, don’t ignore this.
Now, you know, Julie, I’m glad we talked about this topic. Not everybody likes to talk about it. They don’t like to think about checking out their bowel movements afterwards to see, but again, that’s the Bristol [Stool Chart], and that’s very useful.
And now I want to tell everybody, we’ve had Julie on several times. If it’s the first time you’ve seen her, you need to check her out on MyVillageGreen.com on the Humanized podcast. But she can be reached directly at JulieAnnWellness.com. That’s Ann without an E. So that’s J U L I E A N N wellness, W E L L N E S S.com. You’ll see a lot of information there. And do you do telemedicine, Julie?
Julie Davey: I do. My practice is completely virtual. So I work with clients really all over the world. I have clients in other countries and all over the U.S. So, yeah, reach out to me. I’d be happy to answer any questions. I also offer 15-minute free discovery calls. If you have questions, or if you want to see if it would be a good fit to work together, then we can certainly arrange that. So, yeah.
David Stouder: Well, and this is why we do this, and we thank Village Green for sponsoring us because, besides the supplements and all this, we have good staff and we want to bring some of these leading thought leaders like Julie Davey to you for free because, we like to think our typical MDs are our health coaches, and I don’t say this in a critical way, but they’re kind of not. They’re very good at disease management symptoms and diagnoses, but I haven’t met too many that have a real handle on nutrition and things like that. So to me, having a good nutritionist, a good health coach, somebody, is just hand-in-hand. And don’t let these little chronic things just fester and then you get a real problem.
And Julie, thanks again for being with us. We really appreciate you.
Julie Davey: Yes. Thank you for having me.









